Specialists in private practice have been hit hard by COVID-19, with new Australian data revealing they are battling plummeting patient numbers, falling income and rising stress levels as a result of the pandemic.
More than half of private specialists have relied on the Federal Government JobKeeper scheme to support practice staff and one in 12 predict their practice could close or be sold in the next six months, according to new data from the long-running MABEL (Medicine in Australia: Balancing Employment and Life) survey.
A new report, The impact of COVID-19 on GPs and non-GP specialists in private practice, draws on an online survey of 2235 GPs and non-GP specialists conducted in mid-May to reveal the wide-reaching impacts of the pandemic on doctors’ workloads, income, stress levels and practice organisation.
Falling income
Four in five specialists reported their monthly income fell in May compared to before the pandemic, with the figure even higher among surgeons and anaesthetists (94%), due to the cancellation of non-urgent elective surgery across Australia.
One third of surgeons and anaesthetists said their monthly income was cut by more than 50%.
Patient numbers plummet
While 76% of specialists made use of using MBS-funded telehealth consults, almost four in five saw patient numbers drop. The average weekly patient load was just 35 patients in May 2020 – down from 56 patients per week reported in the 2018-19 survey data.
Only 7.1% of specialists reported an increase in patient numbers compared to before the pandemic.
Medicare data also reflect the reduction in patient demand, with a 34% fall in operations, a 43% fall in face-to-face attendances, and even after the introduction of new telehealth items, a 15% drop in total specialist attendances in April compared to March 2020.
The fall in patient demand saw specialists work less – an average of 35.4 hours per week in May 2020, compared to 41.9 hours per week reported in 2018-19.
Stress more common
However, stress levels increased, with 61% of specialists and GPs reporting feeling stress more often than usual between mid-April and mid-May.
Overall, 6.5% of specialists said they felt very financially stressed and a further 20.6% felt moderately financially stressed about their private practice due to the pandemic. Those in large private practices were the most likely to be affected by financial stress.
 Changes in practice operations
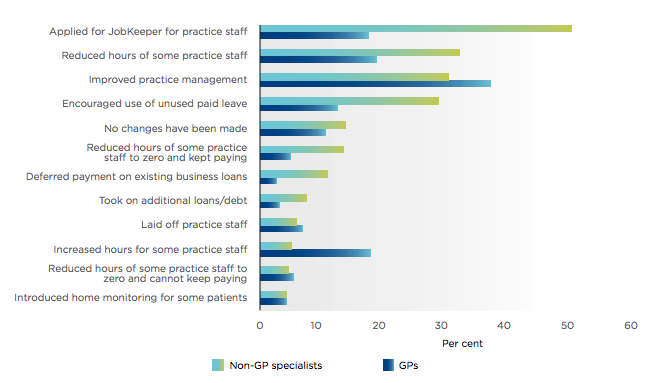
Changes in practice operations