
Dr Davina Buntsma. Source: RACP
Doctors are leaving the RACP’s specialist training programs because they don’t allow enough flexibility for family planning, the college’s trainee committee chair says.
Dr Davina Buntsma says she has also heard from specialist trainees who felt compelled to have fewer children than they wished due to restrictive and outdated rules for registrars.
“Parental leave is currently limited to two years per training program,” she told the RACP congress in Melbourne last week.
“One trainee had planned to have four children but was only able to have two due to the time limit on allowable leave.”
“This is our reality, many trainees are limiting their family size to accommodate training.”
Dr Buntsma, an adolescent health fellow at the Royal Children’s Hospital in Melbourne, called for a root and branch reform of the college’s parental leave policies.
This was increasingly important given that training coincided with the time many doctors were seeking to start a family, with the average basic trainee commencing at 31 and advanced trainees typically starting at 34, she said.
While almost 60% of the roughly 1,400 doctors entering basic training each year were women, the program had a long way to go to become family friendly, Dr Buntsma said.
She said it was common for trainees to have to cut short their parental leave and return to full-time work to meet the rotational requirements of basic training.
Dr Buntsma quoted one doctor as saying: “I feel really sad about missing this time with my children and worried about the pressure it will place on our family unit.”
“I’m also worried about providing the best care for my patients when I’m trying to juggle so much. I’m thinking about leaving the program.”
Dr Buntsma added that she had seen female trainees discriminated against for needing to attend medical appointments for IVF, including being told that training was “not an appropriate time to be undergoing this or planning pregnancy due to work demands.”
“As a female trainee who may want to take time off to have a baby, it makes it much harder if you fall pregnant, then risk pulling out of a 12-month position and burning bridges with future employers.”
“The reality is that rural rotations are also separating families for significant periods of time.”
The message followed research which found half of female doctors in Australia and New Zealand had experienced pregnancy complications and were also more likely to miscarry than other women.
The study, presented at the Royal Australasian College of Surgeons annual scientific congress this month, found 36% of female doctors had experienced at least one miscarriage. The rate in the general population was 20-25%.
More than 60% of the 1099 doctors in the survey also reported delaying family planning due to work reasons.
The median age for a female doctor’s first child was 32, almost three years higher than the general population.
Lead author Dr Jasmina Kevric, a surgical registrar at Northern Hospital in Melbourne, said the results highlighted the need for cultural change.
“Long working hours increase the risks of neonatal complications, while options for part-time training are limited and only suit those in early pregnancy,” she said.
“In the past seven years I have not come across one pregnant [surgical] registrar.”
How each specialty stacks up on gender
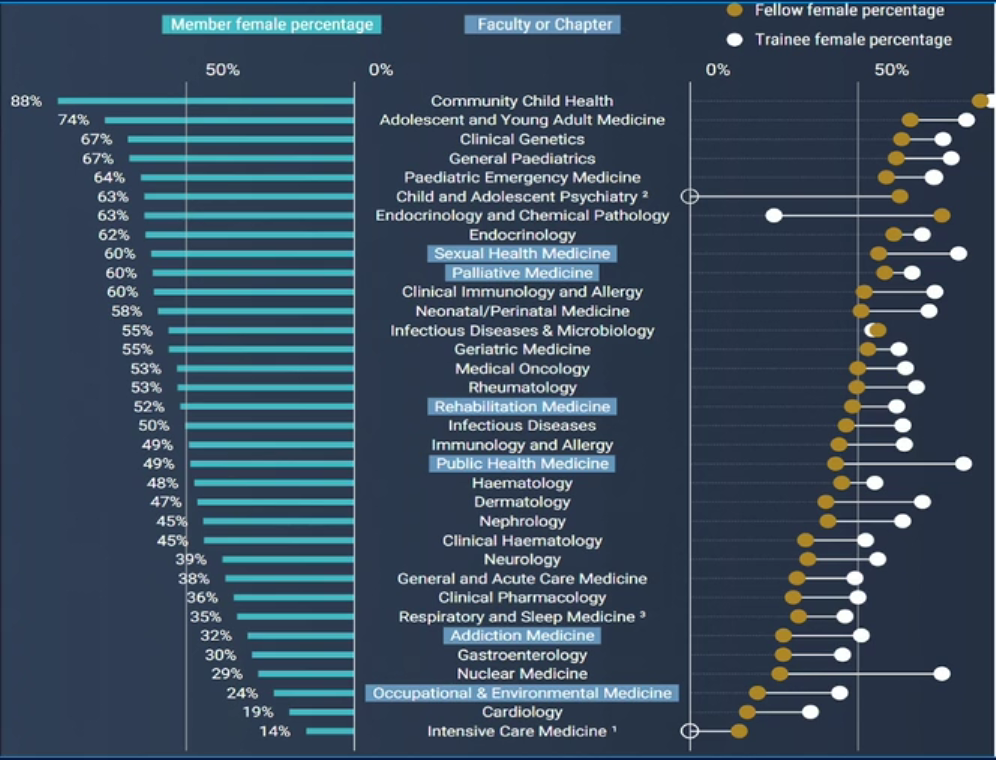
Source: RACP Congress 2022