
Professor Daniel Steinfort
Systematic endoscopic mediastinal staging in patients with locally advanced NSCLC provides more accurate information on the extent of disease than staging by PET alone, new research shows.
The Australian-led international SEISMIC study published in The Lancet Respiratory Medicine [link here] found systematic endoscopic staging commonly downstaged disease from initial PET staging but also identified PET-occult disease.
The single-arm study, conducted at seven tertiary lung cancer centres in Australia, Canada, the Netherlands, and the US, enrolled 155 adults with suspected or known locally advanced NSCLC based on CT and PET findings.
All were considered potential candidates for radical dose or high-dose palliative conventional radiotherapy with or without chemotherapy.
Patients underwent endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) with systematic examination of mediastinal lymph node stations.
Lymph nodes were determined EBUS-positive if cytological examination of needle aspirates showed malignancy. Benign or inadequate specimens were determined EBUS-negative.
The study, led by Royal Melbourne Hospital’s Head of Interventional Pulmonology Professor Daniel Steinfort, found discordant staging between PET and EBUS-TBNA in 37% of patients.
The primary outcome of PET-occult lymph node metastases was identified in 12% of patients, particularly in patients with clinical stage IIIA or cN2 NSCLC.
Contralateral PET-occult N3 disease was identified in 7% of patients.
The study said identification of PET-occult disease impacted treatment planning.
Twelve patients received definitive chemoradiotherapy with extended target volumes, two received high-dose palliative radiotherapy with expanded treatment fields, and one patient received chemotherapy after upstaging from T4cN0 to T4N3, followed by chemoradiotherapy.
“The remaining three patients were precluded from radiotherapy on the basis of excessive toxicity risk following expansion of treatment fields and received systemic therapy or best supportive care.”
As well, in silico radiation studies showed that patients with PET-occult disease would have received a suboptimal radiotherapy dose if planned based on PET results alone.
Downstaging
The study said EBUS identified less extensive mediastinal disease than PET in 39 participants (25%).
“Of these, 31 (20% of cohort [14–26]) were down-staged from cN2–3 to cN0–1. 20 of these 31 patients underwent resection, with post-operative staging confirming EBUS-TBNA findings in all patients (16 patients with pN0 and four with pN1),” the study authors said.
“Accurate down-staging of PET-positive mediastinal lymph nodes can inform selection of patients for curative intent resection,” the study concluded.
The findings support the use of systematic endoscopic lymph node staging in all patients before definitive radiotherapy to most accurately define disease extent and guide optimal management.
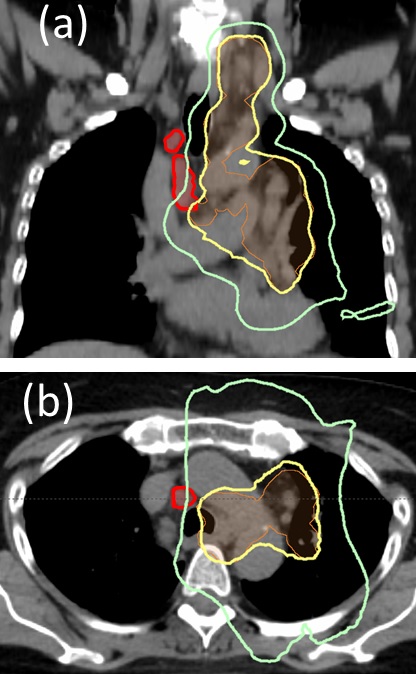
Coronal (A) and axial (B) CT images from a representative patient
with EBUS-detected PET-occult N3 lymph node metastases.
PET-occult lymph node metastases (red) are positioned outside the radiotherapy planning target volume (orange), and outside the desired dose (57 Gy, 95% of the prescription dose, yellow). A large proportion of PET-occult tumour volume receives less than 50% of the desired dose (green)
Professor Steinfort told the limbic the study’s findings will direct practice in this group of patients with locally advanced lung cancer towards a much more thorough evaluation of the lymph nodes in their chest.
“And the reason for that is that about 12% of patients have what we call PET-occult disease… and if the radiation fields are constructed purely on the PET-based information in those groups, then they don’t have those sites of disease included in the radiation field and their likelihood of disease recurrence is almost 100%.”
He said implementation of EBUS-TBNA staging into routine practice required very little extra resourcing.
“Most patients will have an EBUS procedure as their diagnostic procedure and so really, all they’re having is a procedure that requires slightly more thorough lymph node sampling than is routinely done.”
“Probably all tertiary hospitals have an EBUS service because it’s such a standard technique in assessment of intra thoracic lesions so it’s a strategy that should be able to be implemented almost immediately without extra infrastructure or costs.”
“We hope that the strength of the findings will convince people that it’s an important thing to be making a routine aspect of clinical care.”
An accompanying Comment article in the journal [link here] said the study represented “a step in the direction of high-precision radiotherapy centred on the necessity of tissue confirmation of involved and non-involved mediastinal lymph nodes in patients with locally advanced NSCLC.”
However, it also said: “The clinical impact of lack of treatment of unforeseen positive mediastinal lymph nodes is controversial given the high risk of distant relapses in patients with locally advanced NSCLC.”
“In the future, surrogate biomarkers (eg, circulating tumour DNA, molecular profile, and PDL1 status) or higher technology imaging might further refine selection of higher-risk patients with unresectable locally advanced NSCLC.”