The emphasis on the differences between therapeutic agent for COPD may be misplaced if the drug isn’t actually getting to where it’s needed, and there are calls for more focus on choosing the device. This was the message at a sponsored symposium, held during the 2019 European Respiratory Society (ERS) Congress: “Putting the patient needs first: Time for optimising treatment and device selection”.
Choose the device first: Challenging the current prescribing paradigm
When treating a patient with COPD, the choice of therapeutic agent should be secondary to choosing a suitable inhaler device for that patient, suggested symposium presenter Doctor Omar Usmani from the National Heart and Lung Institute, Imperial College London & Royal Brompton Hospital. “You need to have the right device to get the drug into the right part of the lungs,” he said.
When choosing a device, both patient factors and device characteristics are important considerations, Doctor Usmani explained. The patient’s peak inspiratory flow rate, inhaler technique and level of adherence should be assessed alongside aspects of the device design and engineering, including whether the device can deliver a high fine particle fraction, its aerosol velocity, and its internal device resistance.
Tailoring the device to the patient
A management algorithm was developed by Doctor Usmani in collaboration with a multidisciplinary team of healthcare professionals to guide physicians on the choice of an appropriate inhaler device before then choosing the drug formulation.1 The algorithm recommends assessing whether patients can inhale quickly and deeply. If they can do this, it’s more likely that they can generate the peak inspiratory flow required for optimal delivery from a dry powder inhaler (DPI) device.2 However, patients who are unable to inhale like this and instead have a slow and steady style of inhalation would be more suited to a pressurised metered dose inhaler (pMDI) or soft mist inhaler (SMI), according to the algorithm.1
Peak inspiratory flow rate: an important consideration with DPIs
Doctor Mahler, Emeritus Professor of Medicine at Geisel School of Medicine at Dartmouth, Hanover, New Hampshire, described to symposium delegates the significance of peak inspiratory flow rate (PIFR) in relation to the use of DPIs. He explained, “Patients need to create turbulent energy to disaggregate the drug particles from the carrier – usually a lactose particle – to get small 5 µm [in diameter] or less particle size.” The disaggregation takes place inside the inhaler device, and the effect is increased if the acceleration is fast at the start of inhalation.2
The inspiratory force needed to disaggregate and disperse the dry powder differs between DPIs, according to the device’s unique internal resistance.3 An observational study found that up to 40% of patients showed ‘discordance’ with prescribed DPIs, meaning that the patient’s measured PIFR was not sufficient for the resistance of the device they were prescribed.3
Observational studies have also found that up to half of all patients with COPD have PIFRs below 60 L/min, which is considered suboptimal.2 Further, PIFR has been shown to decrease as disease severity increases.4
While there are limited studies investigating the clinical effect of suboptimal PIFR in patients using DPIs, a single-centre retrospective analysis of hospitalised patients with COPD found that suboptimal PIFR was associated with readmissions within 90 days.5 The authors report, “PIF was the only variable (P = 0.041) that predicted days to COPD readmission in a multivariate model incorporating age, sex, percent predicted FEV1, Charlson Comorbidity Index, and inspiratory flow group.” The authors concluded that suboptimal PIFR is common in patients with acute exacerbation of COPD and predicts all-cause and COPD admissions.5
Targeting therapy to the site of airway limitation
In its definition of COPD, The Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease (GOLD)6 explains, “The chronic airflow limitation that is characteristic of COPD is caused by a mixture of small airways disease and parenchymal destruction (emphysema), the relative contributions of which vary from person to person.”
This small airways dysfunction is present in the majority of patients with COPD, progressively increases with GOLD classifications and is closely related to the high impact of disease on health status,7 said Dr Usmani. Therefore, he said, it’s important to consider whether the inhaled drug is actually reaching the small airways to allow it to exert its therapeutic effect.
“A high fine particle fraction (particles that are less than 4.7 um) achieves better lung deposition and large and small airways deposition,” Dr Usmani explained. He described the results of a study that compared lung deposition of three particle sizes of inhaled salbutamol sulphate in COPD (1.5, 3, and 6 µm) at two different inhalation flows (fast: >60L/min and slow: >30L/min). “Striking differences in the deposition behaviour of different sized drug particles exist within COPD airways. Small aerosol particles inhaled slowly are able to penetrate to all parts of the lungs,”8 the study authors report.
Different inhaler devices vary in their ability to deliver drug to the small airways.9 The results of one study that compared tiotropium bromide delivered via a dry powder inhaler (Handihaler) and slow mist inhaler (Respimat) illustrate how this can have an impact on treatment effect. Only the slow mist inhaler significantly improved small airway function in the study population (44 COPD patients, mean FEV1 = 68% pred). It also significantly improved large airway FEV1. The investigators concluded, “This is the first study to show the inhaler device matters in targeting drug to the site of airflow limitation in COPD.”9
The Respimat is a soft mist inhaler that delivers a high fine particle fraction with a slow aerosol velocity.10 The fine particle fraction is around 2.5 times higher than those delivered via pMDIs and the velocity is around five times lower, contributing to an improved lung deposition.10
Referring to the data illustrating the improved pulmonary drug delivery with the Respimat inhaler device, Dr Usmani told delegates that device choice should be a key consideration when treating patients with COPD. He noted, “We have the ability to target the drug to where the pathologists and physiologists have told us for years is where the problem is…with a device that can send the drug to both large and small airways.”
Abbreviations: COPD; chronic obstructive pulmonary disease; DPI: dry powder inhaler
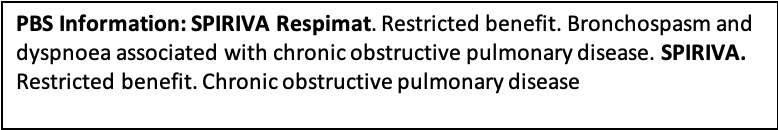
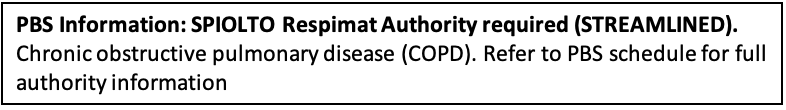
Please review Product Information before prescribing. Full Product Information is available at www.boehringer-ingelheim.com.au/pi
RESPIMAT® is a registered trademark of Boehringer Ingelheim. Boehringer Ingelheim Pty Ltd.
ABN 52 000 452 308. 78 Waterloo Road, North Ryde, NSW 2113. PC-AU-101160. Date of preparation February 2020
References
- Usmani O et al. Choosing an appropriate inhaler device for the treatment of adults with asthma or COPD. Available at guidelines.co.uk https://www.guidelines.co.uk/respiratory/inhaler-choice-guideline/252870.article
- Mahler D. Peak inspiratory flow rate as a criterion for dry powder inhaler use in chronic obstructive pulmonary disease. Ann Am Thorac Soc 2017; 14(7):1103–1107 https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201702-156PS
- Ghosh S et al. Prevalence and factors associated with suboptimal peak inspiratory flow rates in COPD. Int J COPD 2019;14:585–595 https://www.ncbi.nlm.nih.gov/pubmed/30880948
- Prime D et al. Effect of disease severity in asthma and chronic obstructive pulmonary disease on inhaler-specific inhalation profiels thorugh the ELIPTA dry powder inhaler. https://www.ncbi.nlm.nih.gov/pubmed/26372467
- Loh CH et al. Suboptimal inspiratory flow rates are associated with chronic obstructive pulmonary disease and all-cause readmissions. Ann Am Thorac Soc 14(8):1305–1311. https://www.ncbi.nlm.nih.gov/pubmed/28406710
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2020 report. https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
- Crisafulli E et al. Prevalence of small-airway dysfunction among COPD patients with different GOLD stages and its role in the impact of disease. Respiration 2017;93:32–41 https://www.ncbi.nlm.nih.gov/pubmed/27852080
- Biddiscombe M et al. Drug particle size and lung deposition in COPD. Eur Resp Journal 2016;48:PA313. https://erj.ersjournals.com/content/48/suppl_60/PA313
- Biddiscombe M et al. Efficacy of the device in targeting tiotropium to the small airways in COPD. Eur Resp J 2018;52:PA1017;DOI:10.1183/13993003.congress-2018.PA1017 https://erj.ersjournals.com/content/52/suppl_62/PA1017
- Zierenberg B. Optimizing the in vitro performance of Respimat. J Aerosol Med 12 (S19). https://www.ncbi.nlm.nih.gov/pubmed/10623337