Neurologist Dr Javier Pagonabarraga Mora from Spain recently visited Australia to meet with neurologists and present his views on the interplay of both dopaminergic and non-dopaminergic circuits in the pathophysiology of Parkinson’s disease (PD).
Dr Pagonabarraga Mora is from the Movement Disorders Unit at Sant Pau Hospital, Barcelona. He presented data supporting his view that while L-dopa remains the most efficacious dopaminergic drug available for PD, its association with motor fluctuations and dyskinesias makes it important to treat with the lowest possible doses to limit the risk of dyskinesias. “To delay L-dopa therapy has no protective effect on the development of motor fluctuations and dyskinesias, but it is important to treat with as low doses of L-dopa as possible to manage functional disability,” he said. “The use of dopamine agonists helps lower the dose of L-dopa throughout the course of Parkinson’s disease,”1 he added, but noted that these drugs are associated with ‘non-motor’ side effects, including impulse control disorders, somnolence, constipation, dizziness, hallucinations and nausea.2 He suggested that a range of mechanisms of action are needed to limit the total L-dopa daily dose and to avoid adverse events. “It is not important which is the first dopaminergic drug to use, but the total L-dopa dose achieved during the first years of treatment [is important],”3 he said.
Management of PD motor symptoms beyond L-dopa
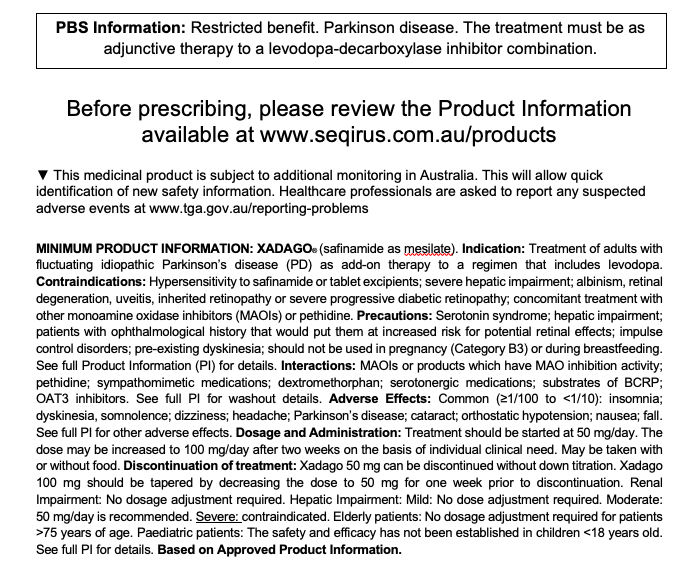
Safinamide (Xadago) is indicated in Australia for fluctuating idiopathic PD as add-on therapy to L-dopa.4 Its activity includes selective, reversible monoamine oxidase type B inhibition, sodium channel blockade, calcium channel modulation, and inhibition of glutamate release in areas of glutamate hyperexcitability, although it’s unknown whether these mechanisms are relevant to its use in humans.4
Dr Pagonabarraga Mora presented in vivo data supporting the role of overactive glutamatergic neurotransmission in the development of L-dopa induced dyskinesias5,6 and a neurophysiological study of safinamide (100 mg/day) showing a restoration of the abnormal cortical facilitation in the primary motor cortex – an abnormality Dr Pagonabarraga Mora considered to be a possible contributor to the pathophysiology of L-dopa induced dyskinesias.5
Improvement in motor and non-motor fluctuations with safinamide
Dr Pagonabarraga Mora took the audience through data illustrating the impact on motor and non-motor fluctuations of safinamide when added to levodopa and other PD therapy.7-11
In a phase 3 double-blind study, patients on stable levodopa plus benserazide or carbidopa therapy (n=549)7 were randomised to adjunctive safinamide (starting dose of 50 mg and increased to 100 mg if tolerable) or placebo for 24 weeks. All patients had idiopathic PD with off time of greater than 1.5 hours a day (excluding morning akinesia).7
The primary outcome was mean change from baseline to week 24 in daily ON time (relief of parkinsonian motor features without troublesome dyskinesia). At week 24, mean (±SD) change in daily ON time was +1.42 (±2.80) hours from baseline (9.30 ±2.41 hours) for safinamide and +0.57 (± 2.47) hours from a baseline (9.06 ± 2.5 hours) for placebo (least-squares mean difference, 0.96 hour; 95% CI, 0.56 – 1.37 hours; P<0.001). The most frequently reported adverse event was dyskinesia, which was expected due to increased dopaminergic stimulation (40 [14.6%] for safinamide versus 15 [5.5%] for placebo). The authors conclude, “The outcomes of this trial support safinamide as an effective adjunct to levodopa in patients with PD and motor fluctuations to improve on time without troublesome dyskinesia and reduce wearing off.”7
These results confirm the findings of an earlier phase 3 double-blind, placebo-controlled trial evaluating the safety and efficacy of safinamide as add-on therapy to L-dopa in patients with PD and motor fluctuations.8 Patients were randomised to oral safinamide 100 mg/day (n=224), 50 mg/day (n =223), or placebo (n = 222) for 24 weeks.
At week 24, increases (mean ± SD) in the total ON time with no or non-troublesome dyskinesia (the primary outcome measure) were 1.36 ± 2.625 hours for safinamide 100 mg/day, 1.37 ± 2.745 hours for safinamide 50 mg/day, and 0.97 ± 2.375 hours for placebo. Least squares mean differences in both safinamide groups were significantly higher versus placebo (p= 0.0223 for safinamide 50mg; p=0.0130 for safinamide 100mg). Improvements in OFF time, motor scores (UPDRS Part III), clinical global impression of change (CGI-C) were all significantly higher for both safinamide groups compared to placebo. There were no significant differences for incidences of adverse events between the groups. The authors say these results indicate, “Safinamide improves motor symptoms and parkinsonism without worsening dyskinesia”.8
The majority of randomised patients (81%) continued into an 18-month extension study9 with a primary end point of a change in Dyskinesia Rating Scale (DRS) total score during ON-time over 24 months (n=544). The study found no significant differences between the safinamide and placebo groups for change in DRS, although ad hoc subgroup analysis of moderate to severe dyskinetic patients at baseline (36% of patients) showed a decrease with safinamide 100 mg/day compared with placebo (p=0.0317).
A post-hoc analysis of data from the phase 3 and extension study investigated the effects of safinamide on mood.10 It found that safinamide significantly improved the Parkinson’s Disease Questionnaire (PDQ-39) ‘Emotional well-being’ domain after 6 months (p = 0.0067) and 2 years (p = 0.0006) compared to placebo. There were also improvements in the GRID Hamilton Rating Scale for Depression (p = 0.0408 after 6 months; p = 0.0027 after 2 years). In addition, significantly more patients in the placebo group experienced depression as an adverse event (p = 0.0444 after 6 months; p = 0.0057 after 2 years). The authors suggested, “The favourable effect of safinamide on mood may be explained by the improvement in wearing off and by its modulation of glutamatergic hyperexcitability and reversible MAO-B inhibition.” They recommend further studies to investigate this potential benefit.10
In a more recent study (published in 2021),11 investigators retrospectively analysed the data of patients (n = 82) at one and three months follow-up compared to baseline for the effects of safinamide on depression and motor symptoms in patients with Parkinson’s disease. Safinamide led to an improvement in depression (Hamilton Depression Rating -6 ± 5.10 at 1 month and -7.27 ± 5.10 at 3 months, p<0.0001) and significant improvement in daily life activities and motor symptoms/motor complications on the Unified Parkinson’s Disease Rating Scale domains II, III and IV. Serotonin syndrome was not observed in patients taking concurrent antidepressants (n = 44), although some isolated serotonin syndrome symptoms were observed within the study population.11
Dr Pagonabarraga Mora presented the results of a recent open-label prospective study investigating the effect of safinamide on non-motor symptoms of Parkinson’s disease.12 The primary outcome measure was change from baseline at 6 months in the non-motor symptoms scale (NMSS) total score. At 6 months, 44 of 50 patients had completed the follow-up. NMSS total score was reduced by 38.5% (from 97.5 ± 43.7 to 59.9 ± 35.5, p<0.0001). Improvements were made in the domains of sleep/fatigue (p = 0.002), mood/apathy (p<0.0001), attention/memory (p = 0.026), gastrointestinal symptoms (p = 0.010), urinary symptoms (p = 0.003), and pain/miscellaneous (p < 0.0001). Quality of life was also improved, with a 29.4% reduction in the PDQ-39SI scale (p<0.0001). Dyskinesias and nausea were the most frequent adverse events, occurring in 6% of patients.12
In conclusion, Dr Pagonabarraga Mora said the data showed that, “Safinamide is not only able to improve motor and non-motor fluctuations, but improves good ON time and improves depressive symptoms and associated pains.”
Disclosure
This article was commissioned by Seqirus. The content is based on studies and the author’s opinion. The views expressed do not necessarily reflect the views of the sponsor. Before prescribing please review the Xadago product information via the TGA website. Treatment decisions based on these data are the responsibility of the prescribing physician.
References
- Katzenschlager R et al. Fourteen-year final report of the randomized PDRD-UK trial comparing three initial treatments in PD. Neurology 2008; 71: 474–480
- Stowe RL Dopamine agonist therapy in early Parkinson’s disease. Cochrane Database Sys Rev 2008; Apr 16;(2):CD006564
- Cilia R et al. The modern pre-levodopa era of Parkinson’s disease: insights into motor complications from sub-Saharan Africa. Brain 2014; 137; 2731–2742.
- Xadago Australian Product Information 2022
- Guerra A et al. Abnormal cortical facilitation and L-dopa-induced dyskinesia in Parkinson’s disease. Brain Stimul 2019; 12(6): 1517–1525
- Gardoni F.A critical interaction between NR2B and MAGUK in L-dopa induced dyskinesia. J Neuroscience 2006; 26: 2914 – 2922
- Schapira A et al. Assessment of safety and efficacy of safinamide as a levodopa adjunct in patients with Parkinson disease and motor fluctuations: A randomised clinical trial. JAMA Neurology 2017; 74(2): 216 – 224
- Borgohain R et al. Randomized trial of safinamide add-on to levodopa in Parkinson’s disease with motor fluctuations. Movement Disorders 2014; 29(2): 229–237.
- Borgohain R et al. Two-year, randomized, controlled study of safinamide as add-on to levodopa in mid to late Parkinson’s disease. Movement Disorders 2014; 29(10): 1273–1280.
- Cattaneo C et al. Long-term effects of safinamide on mood fluctuations in Parkinson’s disease. Journal of Parkinson’s Disease 2017; 7: 629–634.
- Pena E et al. Impact of safinamide on depressive symptoms in Parkinson’s disease patients (SADness-PD study): A multicentre retrospective study. Brain Sci 2021; 11:232
- Garcia DS et al. Safinamide improves non-motor symptoms burden in Parkinson’s disease: An open-label prospective. Brain Sci 2021; 11(3):316; https://doi.org/10.3390/brainsci11030316