 The NSW Telestroke service has assessed its 200th patients since its March 2020 launch and is on track to cover 23 hospitals within two years.
The NSW Telestroke service has assessed its 200th patients since its March 2020 launch and is on track to cover 23 hospitals within two years.
The service is delivered via a statewide virtual hospital that specialises in stroke assessment and treatment, allowing the referring hospital’s emergency staff to consult with a specialist stroke neurologist via the statewide unified communications platform.
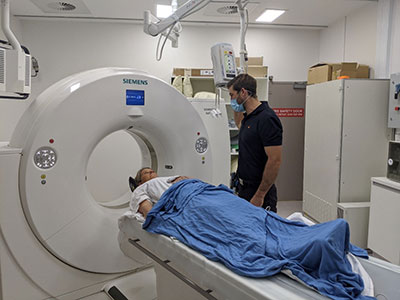
Based at the Prince of Wales Hospital, Sydney, the centralised multi-modal imaging is accessible for all sites via the statewide Enterprise Imaging Repository (EIR), which allows specialists in regional locations to review and assess a patient’s brain scans in a secure environment at any time.
“Centralised imaging is a critical component of the NSW Telestroke service. Diagnostic and treatment decisions are based on acute stroke images,” says Professor Ken Butcher, Medical Director, NSW Telestroke Service Prince of Wales Hospital.
“Rapid access to the actual brain images, including advanced processed blood flow maps, is an essential part of the clinical workflow. The centralised approach has the additional advantage of access to historical images in patients presenting with an acute stroke.”
The Telestroke service is now operating at four regional hospitals, with two more to go live before Christmas.
Its developers say the goal is to give wider access to best-practice treatment for stroke, especially since regional Australians are 19% more likely to suffer a stroke than their metropolitan counterparts.
In the Telestroke model of care, the stroke specialist will decide based on CT scans if the patient is a candidate for thrombolysis and/or endovascular clot removal.
According to NSW Health, a recent case in point involved a woman from Port Macquarie in northern NSW.
Around 9.45pm one evening she noticed that the tingling sensation she had felt earlier in her arm had progressed to weakness and numbness of the arm and side of her face, and problems with her vision. Suspecting a stroke, an ambulance was called and by 10.30pm she was in Port Macquarie Hospital.
A call was made to the Telestroke service, who then contacted Dr James Evans, a neurologist specialising in stroke and neurovascular imaging, 315km away at Gosford Hospital.
Using Telestroke, Dr Evans shared screens with Port Macquarie Hospital via the EIR system to view the scans. Once Dr Evans had assessed the scans, he prescribed thrombolytic therapy for the patient.
After she underwent thrombolytic therapy, she was transferred by fixed-wing aircraft to John Hunter Hospital in Newcastle where a surgical procedure to remove the clot blocking her brain artery was performed by Dr Ferdinand Miteff, a neurointerventionist.
Two days after the successful procedure, the patient was transferred back to Port Macquarie Hospital where she was subsequently discharged three days later.