Multiple myeloma is a heterogenous disease with variability in the presentation of its cytogenetic, molecular and proliferative features. But the treatment of multiple myeloma, particularly in relapsed disease is even more complex. With a therapeutic landscape that has recently exploded with new agents and label extensions and no one standard treatment, clinicians and patients continue to face choices at every junction.1
At every step, management must be individualised based on many factors which may include a patient’s prior therapy, their duration of response to prior therapy, the rate of disease progression, the patient’s physical fitness and the patient’s attitudes and preferences towards treatment options.1
The result is a plethora of treatment options that may be administered in numerous orders and combinations, but no one standard treatment option to be guided by.1
Although ‘individualised’ treatment seems a hot topic in medicine right now, in multiple myeloma this translates to complex patient management. Hence clinical judgement seemingly transforms clinicians into artists as they navigate each patient’s unique circumstances and journey.
These days that journey can be a long one. Although multiple myeloma remains an incurable disease, the continual increase in the available treatment options is transforming it into a treatable chronic condition.1
As Professor Anthony Schwarer, consultant haematologist at Cabrini Hospital explains in an interview with the limbic, “There were fewer treatment options available when I started out and most patients died within 3 years. Now some of my patients are living 7 to 10 years. I’ve even got one who is seemingly cured and has been in remission for 15 or 16 years.”
While this is to be celebrated, relapse eventually occurs in virtually all patients and some will exhaust all currently available treatment options during their journey with multiple myeloma.1 “In the end, for some it’s the number of treatments patients have access to that limits their survival,” says Prof. Schwarer.
Australia lacks access to treatments available overseas
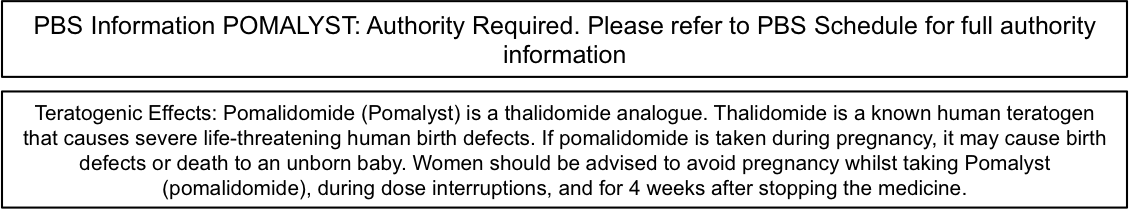
There are a number of treatments listed on the Pharmaceutical Benefits Scheme (PBS) for the treatment of relapsed multiple myeloma, including thalidomide, bortezomib, lenalidomide, pomalidomide, alkylating agents, anthracyclines and corticosteroids – all of which have a proven benefit in clinical trials.1,2
The order and combination of treatments is generally left up to the discretion of the clinician and patient based on the clinical situation and patient choice, with the exception of pomalidomide which is subsidised after patients have failed treatment with bortezomib and lenalidomide.1,2
However, there are many more treatments that are not yet approved or funded here in Australia that may be accessed through the Special Access Scheme under specific circumstances, but when should they be used?
Clinical trials are constantly changing the status quo of treatment in Australia
There have been many multiple myeloma trials over the last few years.3–7
“Given that the number of treatments a patient has access to is so important, clinical trials offer a temporary boost for those who can access them and are therefore preferred by clinicians when they become available. This was the case recently, when relapsed patients had access to clinical trial programs for carfilzomib,”Prof. Schwarer says.
He explains that clinicians in Australia need to be resourceful in maximising the options available to their patients by leveraging access to clinical trials, particularly in relapsed disease: “Usually if there is a clinical trial around and there is no clear reason why the patient shouldn’t go onto it then it’s our default mechanism. It gives patients more options if they choose a clinical trial over PBS-funded treatments.”
He goes on to explain that it’s not that the clinical trials offer something better than the PBS-funded treatments: “We know the PBS-funded options in relapsed disease like pomalidomide work well and will always be there, but the clinical trial may not.”
This is an approach widely accepted and recognised in clinical guidelines, including the Myeloma Australia Clinical Practice Guideline, that offers yet another option for patients.1,8 However, Prof. Schwarer warns, “Although, the more advanced a patient is and the more treatments they’ve had, the less likely they’ll respond to the next one, so that’s another point to consider.”
But clinical trials are not the only avenue to access other treatments. One further option that is available to patients in Australia is Compassionate Access Programs. However, Prof. Schwarer explains in his practice they only play a role after all other PBS-funded and clinical trial options have been trialled: “When we have exhausted PBS and clinical trial options, we go to the compassionate access programs,” says Prof. Schwarer, “Compassionate use is certainly not in the first-line patient, but is yet another avenue when they run out of PBS options.”
Myeloma is in its heyday
The management of relapsed multiple myeloma is complex, and will likely remain that way for some time to come. This is in part due to the ever-increasing number of treatments on the horizon,3–7 and secondly to the flexibility around the order and combination in which many treatments are likely to be used. Despite the complexity, clinicians remain enthusiastic about this disease, “It’s exciting. Myeloma is in its heyday. A lot of research was poured into myeloma some years ago and now we’re all benefitting from all that work that’s been put in,” says Prof. Schwarer.
References:
- Myeloma Australia. Clinical Practice Guideline Multiple Myeloma. V.3 Updated August 2015. Available from: http://myeloma.wordpress-staging.3dc.com.au/wp-content/uploads/sites/2/2015/10/MSAG-Clinical-Practice-Guidelines-V.3-AUG-2015.pdf (accessed 22 December 2016).
- Australian Government Department of Health. Pharmaceutical Benefits Scheme (PBS). Available from: pbs.gov.au (accessed 22 December 2016).
- Ocio EM et al. Leukemia 2014;28(3):525–
- Siegel DS et al. Blood 2012;120(14):2817–
- Lonial S et al. N Engl J Med 2015;373(7):621–
- Jakubowiak A et al. Blood 2016;127(23):2833–
- Raje NS et al. Br J Haematol 2016; article accepted in press. DOI: 10.1111/bjh.14483.
- Mayo Clinic. Treatment of Relapsed Myeloma Mayo Consensus. Available from: https://nebula.wsimg.com/7f32effc77a8c2ab9b34f1d90cbe4959?AccessKeyId=A0994494BBBCBE4A0363&disposition=0&alloworigin=1 (accessed 22 December 2016).
This article was sponsored by Celgene Pty Ltd Melbourne, which has no control over editorial content. The content is entirely independent and based on published studies and experts’ opinions, the views expressed are not necessarily those of Celgene Pty Ltd.