Australia’s first national action plan for IBS aims to deliver in key areas such as MBS funding of faecal calprotectin testing, PBS-subsidised access to new IBD medications for paediatric patients and access to IBD specialist nurses
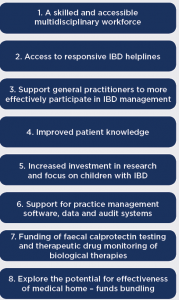
Developed with government support by Crohn’s and Colitis Australia, the plan launched on 24 March outlines eight key priority areas (see diagram) including:
- Establish a minimum of 15 specialist IBD nurse positions in hospital IBD teams.
- Better access to psychologists, dietitians and pharmacists in multidisciplinary team.
- IBD helpline support provided by IBD nurses for patients and clinicians.
- Provision by GPs of IBD personal action plans for flare-ups.
- Implement IBD-specific practice software and quality of care audits.
- Funding of faecal calprotectin testing to discriminate IBD from non-IBD diagnoses, and also potentially for disease monitoring.
- Explore the use of Health Care Homes for IBD patients.
The authors of the report said a national plan was essential given that the prevalence of IBD is increasing and expected to reach almost 100,000 people in 2022.
“Though there have been many advancements in treatment over the last decade and pockets of excellence in care, the burden of disease remains high and the quality of care variable and in many cases does not meet the prevailing standard,” they said.
The report noted that a recent review of IBD care standards found that the 71 hospitals audited did not meet the levels of care specified in the Australian IBD Standards.
“Those living with IBD have expressed the problems that limit their ability to participate actively in their own IBD management,” the authors wrote.
High hospitalisation rates, poor access to multidisciplinary chronic disease care, high psychological impact of living with the disease and inadequate responsiveness to deterioration in care were key problems reported by patients.
Key Priority Areas
The plan was developed based on feedback from a IBD roundtable consultation process that included gastroenterologists Dr Ray Boyapati and Dr Reme Mountifield representing the Australian Inflammatory Bowel Disease Association and GESA, Dr Greg Moore, Head of IBD at Monash Medical Centre and Board Director Crohn’s & Colitis Australia, Dr David Scott (regional gastroenterologist) and Dr George Alex (paediatric gastroenterology).
The four-year action plan is backed by $2 million in funding from Federal government and will be “a step forward in realising the vision of improved quality of life for people living with Crohn’s and colitis,” according to Crohn’s Colitis Australia CEO, Associate Professor Leanne Raven.
“Crohn’s and Colitis Australia … looks forward to collaborating with hospitals, clinics and other medical professionals, alongside the state and territory governments responsible for hospitals, as well as welcoming additional funding to achieve better IBD education for GPs and improve support for children and young people,” she said.