Queensland gastroenterologists have developed a simple risk stratification tool that can detect high‐risk small bowel Crohn’s disease (CD) based on commonly available pathology results in combination with clinical symptoms.
The online tool is ideally suited for primary care as it can accurately identify people with ileal CD based on abnormalities in white cell count, albumin and platelet counts, according to Associate Professor Graham Radford Smith and colleagues at the QIMR Berghofer Medical Research Institute, Brisbane.
 They said there was a need for a simple tool to identify CD in the early stages because delays in diagnosis and specialist referral led to complications and need for surgery. Currently there is no risk stratification tool similar to FOBT for colorectal cancer, and the only available tests such as faecal calprotectin have low sensitivity and high cost making them unsuitable for use in primary care, they wrote in Alimentary Pharmacology and Therapeutics.
They said there was a need for a simple tool to identify CD in the early stages because delays in diagnosis and specialist referral led to complications and need for surgery. Currently there is no risk stratification tool similar to FOBT for colorectal cancer, and the only available tests such as faecal calprotectin have low sensitivity and high cost making them unsuitable for use in primary care, they wrote in Alimentary Pharmacology and Therapeutics.
They therefore investigated the clinical features and biomarkers of ileal CD at first presentation in three cohorts of patients presenting to a gastroenterology clinic, and compared them to control groups referred by GPs but without a diagnosis of CD.
In the first cohort they did a retrospective comparison of a historic group of 61 patients over 18 diagnosed with CD and 78 matched controls without CD. The second cohort was a prospective group of 99 referred patients of whom 42 were found to have CD and 57 had a non-CD diagnosis. The third risk stratification tool was then assessed in a third cohort of 582 additional patients, of whom 87 had a CD diagnosis.
Evaluation of clinical symptoms found that abdominal pain and altered bowel patterns best predicted ileal CD. However when used alone these features had a high false negative rate. When combined with abnormal pathology results for white cell count (WCC), albumin and platelet counts they gave a good prediction of ileal CD (Cohort 2 AUC = 0.96, and Cohort 3 AUC = 0.94). The combination provided a balanced accuracy of 0.82, a sensitivity of 0.88 and a specificity of 0.76. The positive predictive value was 0.71 and negative predictive value was 0.91.
C‐reactive protein was independently associated with ileal CD but non‐signficant in a multivariate model.
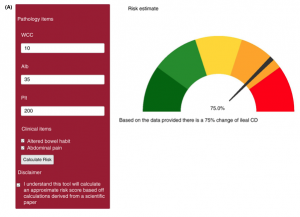
The researchers then used the parameters to develop a prototype online risk stratification tool, which they say could be used by a GP to decide whether a patient presenting with abdominal symptoms should be referred for specialist investigation. They emphasised that the tool was based on high/normal/low pathology results, as opposed to normal vs abnormal, which they said “may yield greater fidelity in ileal CD prediction compared to simply identifying abnormal values.”
They provided an example of a patient whose full blood count and serum biochemistry tests revealed a low albumin, and the values are entered into the risk calculator.
“The patients’ risk of ileal Crohn’s is found to be 75% and this patient is referred on to a gastroenterology service for further urgent investigation,” they wrote.
They acknowledged the tool was based on results from a single centre but said they hoped its use could be explored in practice to overcome the current situation where the diagnosis of CD is typically delayed by an average of two years. They noted that one third of their historical cohort had been diagnosed with CD after an emergency presentation or as an inpatient, suggesting more severe disease.
“The establishment of a simple risk assessment tool for ileal CD will guide clinical decision‐making in the primary care setting,” they said.
“With the increasing diagnostic utility of non‐invasive imaging such as intestinal ultrasound, the presence of a high‐risk score within this tool may warrant preliminary imaging, appropriate urgent referral or an urgent triage category in a population that may otherwise be perceived as low risk.
“These patients may then receive a more targeted assessment and investigations at an earlier timepoint, decreasing diagnostic delay and improving long‐term disease outcomes.”