Consensus guidelines on the management of iatrogenic colonoscopy perforations (ICP) have highlighted the importance of early diagnosis and early initiation of treatment.
The World Society of Emergency Surgery guidelines say iatrogenic perforations are an infrequent but severe complication of colonoscopy, and there have been no guidelines for management until now. They note that while 40-60% of perforations are identified during the procedure, any delay in diagnosis will increase the risk of more invasive treatment such as surgery.
“Physicians should therefore search for this potentially life-threatening complication and run clinical and biochemical tests if an ICP is suspected.”
They state that abdominal pain associated with distension is the most common symptom. When perforation is suspected, minimum laboratory tests should include white blood cell count and C-reactive protein. CT scans are more sensitive than standard radiographs for the detection of free intro-peritoneal air.
The guidelines provide a decision-making algorithm for the management of ICP including conservative management, endoscopic closure and surgery.
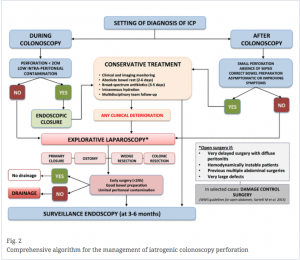
“Endoscopic repair should be attempted whenever the perforation is detected during the procedure, though outcomes depend on the size and cause of the iatrogenic injury, as well as on the operator’s level of experience,” the guidelines say.
The guideline authors found only low-level evidence for the optimal duration of patient observation after conservative or endoscopic treatment for ICP although hospital stays averaged 9 to 13 days.
“It must be stressed that early improvement with conservative treatment does not rule out the potential need for surgery. Close monitoring of the patient will allow detection of clinical deterioration, which may signal the need for emergency surgery.”
“Ideally, these surgeries should occur early and within 24hr of the perforation, as further delays are related to a worse prognosis.”
Short-term antibiotic treatment covering Gram-negative bacteria and anaerobes is recommended following endoscopic closure or conservative management, as is thromboprophylaxis.
The guidelines say the maximum acceptable incidence of ICP is 0.1% in diagnostic colonoscopies and 1% for complex polypectomy.
Patient risk factors for ICP include older age, female gender and low BMI, while the endoscopist’s experience and volume of procedures are also critical.