New guidelines make a strong recommendation against routine use of thyroid hormones to treat subclinical hypothyroidism (SCH) in adults.
Published in the BMJ, the recommendations developed by a panel of international authors including Australian researchers are based on the GRADE approach to evaluating evidence
The main recommendation is that thyroid hormones should not be routinely offered to adults with SCH (elevated TSH levels over 4 mIU/L) and normal free T4 (thyroxine) levels.
“The panel concluded that almost all adults with SCH would not benefit from treatment with thyroid hormones.”
“Instead, clinicians should monitor the progression or resolution of the thyroid dysfunction in these adults,” they recommend.
The guideline authors say their findings are based on a recent major randomised controlled trial and a systematic review of 21 trials that showed thyroid hormones do not improve quality of life or thyroid related symptoms in people with SCH.
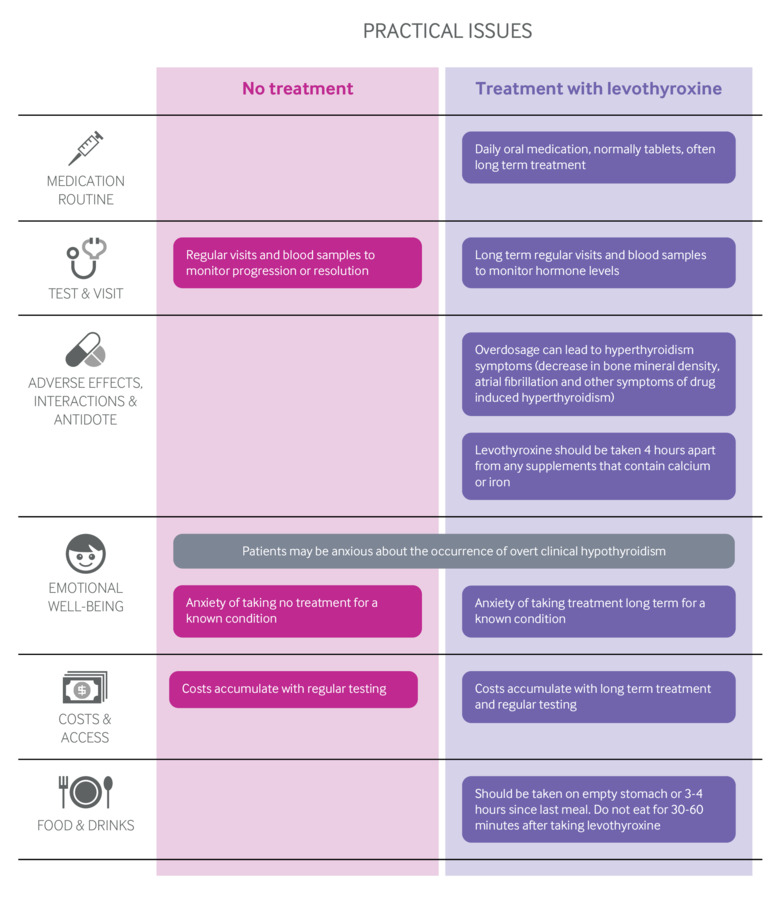
Thyroid hormone treatment imposed a significant lifetime treatment burden on patients and also had risks of adverse effects and overdose, the authors said.
Current guidelines such as those from the American Thyroid Association recommend thyroid hormone treatment be considered for patients with TSH <10 mIU/L, ” if symptoms suggestive of hypothyroidism, positive antibodies to thyroid peroxidase, or evidence of atherosclerotic cardiovascular disease, heart failure, or risk factors for these diseases.”
“If implemented, this recommendation may substantially alter prescribing trends, which show that thyroid hormones are increasingly prescribed, most probably due to SCH,” they wrote.
However they said the recommendation does not apply to women who are trying to become pregnant or patients with TSH >20 mIU/L. And it may not apply to patients with severe symptoms or young adults such as those under 30 years old.
In their review, the authors note that 4-20% of the adult population have SCH, and about one in three patients have no symptoms at all. Non-specific symptoms such as fatigue experienced by many patients with SCH may be due to other conditions, they state.
TSH levels normalise within five years in about 60% of patients with levels between 4 and 10 mIU/L, they add.
“Levels may rise in response to stress and transient disease. This biological variation in TSH values, means that one abnormal TSH level should be followed by a repeat blood test to confirm the diagnosis,” they said.