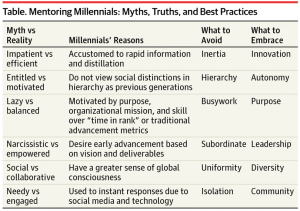
Claims that ‘millennial’ doctors need a different style of mentoring to reflect their generation’s unique communication & working habits have been dismissed as stereotyping and unnecessary.
Writing in JAMA, US surgeon Dr Jennifer Waljee says generational conflicts are now occurring regularly between senior staff mentors and junior doctors who have grown up in an age of instant communication via social media with ‘flat’ hierarchical systems.
She cites examples of mentors who become angry and frustrated at junior doctor mentees who appear impatient, entitled and distracted by their smartphones.
But in many cases these are typical examples of millennials adept at multitasking using technology and social media to rapidly acquire and share information and skills about medicine, according to Dr Waljee who practices at the Michigan Medicine clinic.
Millennials, she says, are accustomed to frequent and rapid interactions from a global network of connections, and are surprised when their mentor does not reply immediately to their email or a senior member of staff shows annoyance at being contacted directly by a junior.
Millennials also baulk at the traditional and slow apprenticeship and peer review system. She cites another example of a millennial doctor wanting to immediately implement and share knowledge of an innovative intervention to improve patient care rather than take the advice of a mentor to wait and develop a clinical trial to generate a high-impact scientific paper.
“A keen awareness of generational mindsets and motivations can allow for more productive and rewarding mentoring relationships, and several strategies can improve intergenerational working relations,” Dr Waljee says.
She suggests solutions such as ‘micromentoring’ with frequent, brief meetings that provide quick yes or no answers on narrow topics. Mentors could also break down the hierarchical communication structures by accepting ‘reverse mentoring’ and using social media platforms such as Twitter to connect with faculty and disseminate research findings.