 Clinicians should put their headsets together and start thinking about how virtual reality can be used to help patients in the oncology setting.
Clinicians should put their headsets together and start thinking about how virtual reality can be used to help patients in the oncology setting.
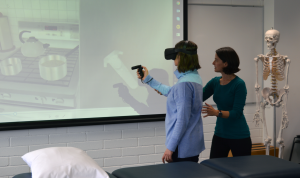
Speaking at the 2019 COSA ASM in Adelaide, Associate Professor Belinda Lange shared some of the types of projects that are already making an impact in other clinical settings.
Associate Professor Lange, a physiotherapist, said some of her work has involved using virtual reality for neurorehabilitation or motivating older adults to exercise.
And with the technology becoming more advanced, more accessible and more affordable, the possibilities to distract, engage, motivate and prepare patients of all ages were limitless.
“We’ve been using virtual reality at the Women’s and Children’s to distract children who are having procedures done and we’ve been using it with adults at the Noarlunga Hospital who are having dialysis,” she told the limbic.
“And so I can see it being really applicable in the cancer area where we have people coming in for procedures whether they be medical procedures or for longer treatments where this type of technology could be used to distract and engage them and take their mind off what is happening.”
She said 360 degree video capture can also be used to create scenarios that can be played back through a virtual reality headset.
“We are doing some work at the moment on a violence prevention program for young males to reduce male on male violence. And so part of that is using 360 degree video to take the user through an experience in which they can test out different scenarios and put different processes into action so they can respond in different ways and find out what the consequences are in a safe environment.”
“And I could see that being used for preparing someone for a procedure. Often the scariest thing about a procedure like radiation therapy or anything that involves a big piece of equipment is knowing what that is going to look like when you get there. So you could take the person through in the safety of the headset and show them what they are going to experience and let them feel the environment and the sounds – and then they are prepared for that when they turn up.”
She said early downsides to using virtual reality – simulator sickness or cyber sickness – were not seen as much now because the technology has improved.
Standard ‘shoot ‘em up’ video games could easily be replaced by content that was more relaxing such as mindfulness apps.
“There are a number that are appropriate for this type of setting and can be used by people of all ages. With the technology catching up, it is really about identifying appropriate content.”
She warned virtual reality should not just be used for its novelty value. It also required co-design or input from end-users and evaluation.
“The important thing to note with any sort of digital technology, but virtual reality in particular, is that we are using it as an adjunct or to enhance clinical care.”
“And where there is a need or gap identified like that, what we do is look for available tools that might be able to be used off the shelf or modified to fill that need or gap.”
She said one of the key barriers to wider application was trying to fit the technologies into the existing health system model.