Specialists’ wages are falling in real terms as growing numbers of new medical graduates enter the workforce and intensify competition for jobs, workforce figures show.
Latest data from the Medicine in Australia Balancing Employment and Life (MABEL) longitudinal study show that growth in specialist medical numbers is ten times that of GP numbers while specialist incomes lag behind inflation.
Some 4,541 new specialists joined the medical workforce between 2011 and 2015, equivalent to an extra 10 full time equivalent (FTE) doctors per 100,000, compared to 1.4 FTE GPs over the same period. Specialist numbers increased ahead of population growth, rising by 1.78% a year over a 10-year period compared to 0.16% growth in GP numbers per year over the same period.
And while expenditure on specialists grew by 4% in real terms between 2014-15 and 2015-16 to $21.2 billion, the average fee per service including Medicare rebate plus out of pocket payment – fell in real terms by 0.15% per year. Specialists’ median hourly earnings (in both public and private sector) grew by just over 1%, which is less than real wage growth in the economy.
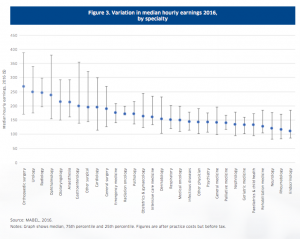
Table courtesy of the ANZ Melbourne Institute Health Sector Report Specialists
The Melbourne Institute Health Sector Report notes that out-of-pocket payments for specialist services continued to grow at 5.5% above inflation, but with substantial variation between what doctors charge within, and between, specialities. The largest variation was seen in surgical and procedural specialities.
“These variations are likely to prompt continued debate around fee disclosure,” writes Professor Professor Anthony Scott from the Melbourne Institute of Applied Economic and Social Research at the University of Melbourne.
Bulk billing rates for specialist attendances grew from 25.7% to 30.7% and from 43% to 44.2% for operations over 10 years. There is also evidence that specialists charge higher fees to their wealthier patients, writes Professor Scott.
Across all the specialities, doctors who worked solely in private practice earned an average of $257 per hour in 2016.
Those working only in the public sector earned $164 per hour, while those working in both averaged $211 an hour.
The report found since 2008, between 62% and 65% of specialists were doing some private practice work.
The report highlights a likely future squeeze on jobs, the direct result of a doubling in medical graduates since the early 2000s that will see increasing competition for coveted specialist training places and consultant positions.
“It is likely to take much longer for these doctors to achieve Fellowship, on top of the 15 years it takes already for some specialties,” Professor Scott predicts, noting not all graduates are making it through the training bottleneck to become specialists.
“Some of these doctors could end up under-employed and working part time when they would prefer to work full-time; or in jobs that do not fully utilise their training; or leaving clinical practice altogether.”
Meanwhile, competitive pressure could also give birth to new corporate business models in specialist practice, “as larger medical groups with more efficient business practices seek to exploit economies of scale”.
“How specialists manage their private sector work could become a key issue,” the report concludes.