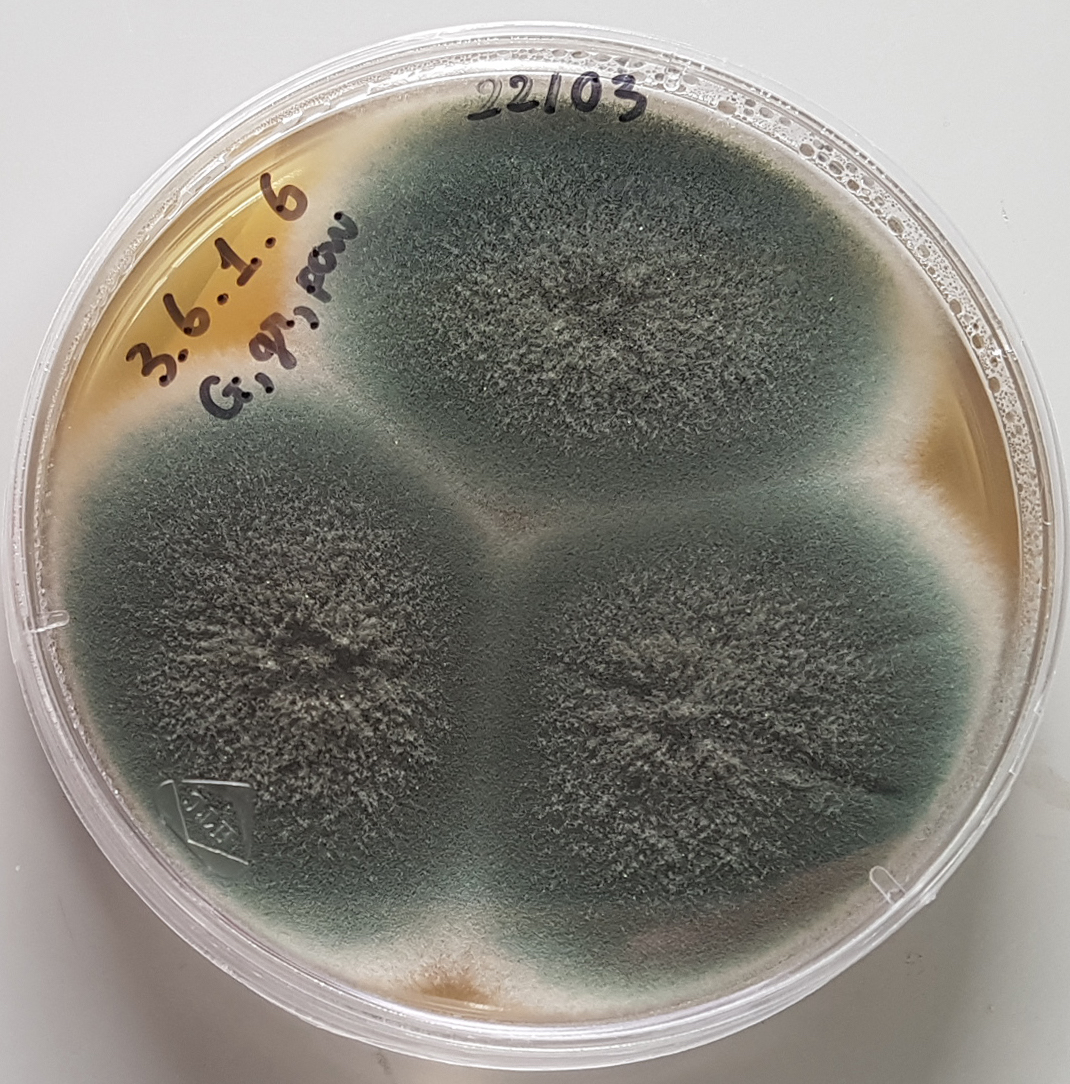
Aspergillus fumigatus
The COVID-19 pandemic, antimicrobial resistance and climate change are conspiring to increase the health risk from pathogenic fungi, especially in people with underlying conditions.
According to a new WHO report, the critical priority fungal pathogens include the respiratory pathogen Aspergillus fumigatus which is becoming increasingly resistant to the azole medications typically used to treat systemic fungal infections.
The report said infections caused by azole-resistant strains kill 47-88% of affected patients. At-risk groups include patients with chronic lung disease, haematological cancers, and bone marrow or solid organ transplant recipients.
Also in the top four critical priority fungal pathogens is Cryptococcus neoformans which has a propensity to infect the brain, especially in immunocompromised individuals.
While the leading risk factor globally is HIV infection, immunosuppression, autoimmune disease, and decompensated liver cirrhosis are other risk factors.
Candida albicans, one the most common fungal pathogens globally, and the newly emerged pathogen Candida auris were also determined to be in the critical priority group.
C. auris is resistant to most antifungal medications and presents a huge treatment challenge for hospitals as affected wards may have to be closed for prolonged periods to avoid transmission between patients.
The report, which included significant contributions from the University of Sydney and other Australian mycoses experts, said cases of invasive fungal disease were rising as at-risk populations including those on immunosuppressive medications continued to expand.
It said the COVID-19 pandemic had also been associated with an increase in comorbid aspergillosis, mucormycosis and candidaemia “with devastating consequences.”
There was also evidence that the incidence and geographic range of fungal disease was increasing due to global warming.
However the emerging global threat from invasive fungal disease was compounded by the rapid emergence of antifungal drug resistance which was partly driven by inappropriate antifungal use, for example in agriculture.
“Currently, only four classes of systemic antifungal medicines (azoles, echinocandins, pyrimidines and polyenes) are currently used in clinical practice, and only a few others are under development.”
“The use of these medicines also required expertise, and drug-drug interactions are particularly common. Such interactions, along with the frequent off-target toxicity and the requirement for lengthy courses of therapy, mean serious adverse events can occur which further impact length of hospitalisation, patient safety and prognosis.”
The report called for improved surveillance of disease and antifungal resistance, targeted support for research and development and innovation in new therapies and diagnostics, and enhanced public health interventions including antifungal medication stewardship.
Fungal pathogens can cause illnesses and death.
They are becoming increasingly common and resistant to treatment.Yet, too little is known about them.
The 🆕 WHO fungal priority pathogens list is an important step to boost urgently needed research:
📌 https://t.co/cXgj2HPZIc pic.twitter.com/4LgdIqf4Lo— World Health Organization (WHO) (@WHO) October 25, 2022
The WHO report identified another seven fungal species of high concern – Nakaseomyces glabrata, Histoplasma spp, Euromycetoma causative agents, Mucorales, Fusarium spp, Candida tropicalis and Candida parapsilosis.
A further eight fungal pathogens ranked as medium priority are Scedosporium spp, Lamentospora prolificans, Coccidioides spp, Candida krusei, Cryptococcus gattii, Talaromyces marneffei, Pneumocystis jirovecii and Paracoccidioides spp.
Pathogens were ranked on the basis of case fatality rate, incidence, geographic distribution, increasing incidence and prevalence, average length of hospital stay, complications and sequelae, antifungal drug resistance, transmission dynamics, access to diagnostic tests and access to evidence based-treatment.
Image of A. fumigatus supplied by the University of Sydney