Shrinking or non-existent Medicare rebates mean cancer patients are now having to pay hundreds and sometimes thousands of dollars for standard radiology tests, advocacy groups say.
Women with breast cancer now face $600 costs for an MRI scan for breast cancer staging and planning because the imaging is not covered by Medicare, a Senate inquiry has been told. And patients with lung cancer are left $258 out of pocket for a PET scans for staging, the Senate’s Community Affairs Reference Committee was told at a public hearing in Brisbane on 13 December.
Patients faced high gap costs for basic imaging tests such as X-rays, CT scans and ultrasound because Medicare rebates have been frozen since 1998, the Australian Diagnostic Imaging Association representative told the inquiry into the availability and accessibility of diagnostic imaging equipment around Australia.
High out of pocket costs also arose because the Medicare system wasn’t keeping pace with imaging technology and rebates had not been approved for many tests that are now considered the basic standard of care, the Association said.
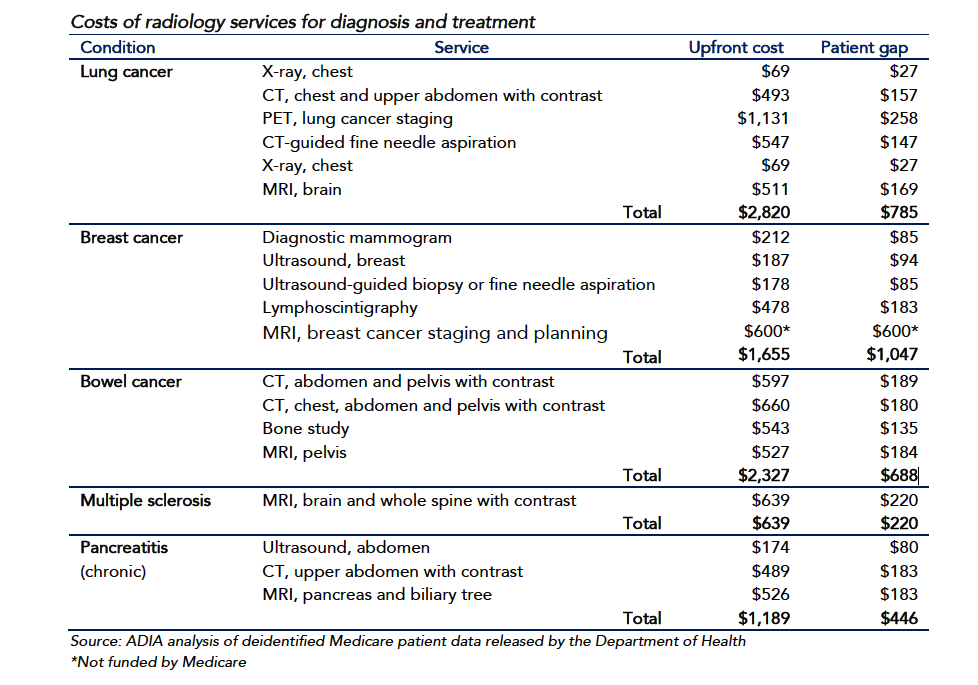
“[Cancers] often require more than one radiology service for diagnosis, treatment and monitoring, meaning that patients pay thousands of dollars upfront and are left hundreds of dollars out of pocket,” the ADIA said in its submission to the inquiry
It cited the example of breast cancer, for which women faced out of pocket costs of $1047 for tests such as diagnostic mammography, ultrasound and lymphoscintigraphy. Lung cancer patients faced upfront payment of $2820 for X-rays, CT scans and PET scans and were left with gap fees of $785.
The claims were backed up by patient advocacy groups, who told the hearing that imaging gap fees were now the major financial burden for cancer patients.
“We know that the financial impact of breast cancer, and of all cancers, is profound and that diagnostic imaging is a considerable cost for people that adds to their distress when they’re diagnosed with breast cancer,” said Danielle Spence of Breast Cancer Network Australia.
She noted there was no Medicare rebate for most women referred to have an MRI as part of their work-up.
“We know they’re paying anywhere from $500 to $1,500 out of pocket for that procedure,” she said.
And inflexible Medicare restrictions such as the “same day rule” for diagnostic breast ultrasound meant a woman was given the choice of paying a large out of pocket cost or returning the next day, the hearing was told.
The same issues were faced by men with prostate cancer said Associate Professor Anthony Lowe, CEO of the Prostate Cancer Foundation of Australia.
“On average, the [out of pocket costs] are in the order of $5,000 to $10,000 for a man over the treatment period but there is currently no Medicare rebate either for multiparametric MRI or for the PET scanning so men are out of pocket in the order of $500 to $600 per scan,” he said
“And that probably is the biggest inquiry we receive from men in our national office. They ask: why is it not rebated? Why do I have to pay this when my clinician is telling me it is essential for me to have this scan in order for them to be able to manage the situation?
Cancer patients can expect gap fees for scans to double in costs over the next decade unless action is taken to unfreeze the Medicare rebates for imaging, the hearing was told.
There was also a need to reform the slow and outdated system of approvals for Medicare rebates, with the Medicare Services Advisory Committee, taking three or more years to consider applications, said Ms Spence.
“By the time these rulings come out, often we’ve moved on to something that’s standard practice overseas,” she said.