This article was commissioned by Bayer Australia Limited.
The second-generation androgen-receptor inhibitors (ARi’s) have shown metastases-free survival (MFS) and overall survival (OS) benefits in patients with non-metastatic castrate-resistant prostate cancer (nmCRPC),1-6 providing treatment options beyond continued androgen deprivation therapy (ADT).
In a Bayer webinar chaired by Doctor Laurence Krieger, lead clinician and principal investigator for numerous studies in urogenital malignancies at the Northern Cancer Institute, Sydney, experts explored some of the latest data for ARi’s and the clinical considerations in using these treatments in men with nmCRPC. The panel included Doctor Neal Shore, who was a lead investigator in the recently-reported ARAMIS trial1,2 for the second-generation ARi darolutamide. The panel also included Professor Declan Murphy from the Peter MacCallum Cancer Centre in Melbourne and Doctor Niara Oliveira from Mater Hospital Brisbane.
MFS and OS benefits with darolutamide: ARAMIS trial
Doctor Shore, Medical Director for the Carolina Urologic Research Centre in the United States, explained that patients with nmCRPC are mostly asymptomatic from their cancer but have rising PSA levels. Although this is an important patient group to manage, he noted that treatment guidance has been limited until now, but the emergence of the benefits of second-generation ARi’s in nmCRPC is rapidly changing the treatment approach.
Doctor Shore provided an overview of the ARAMIS trial results, which were reported this year at the ASCO 2020 and ESMO 2020 virtual meetings.
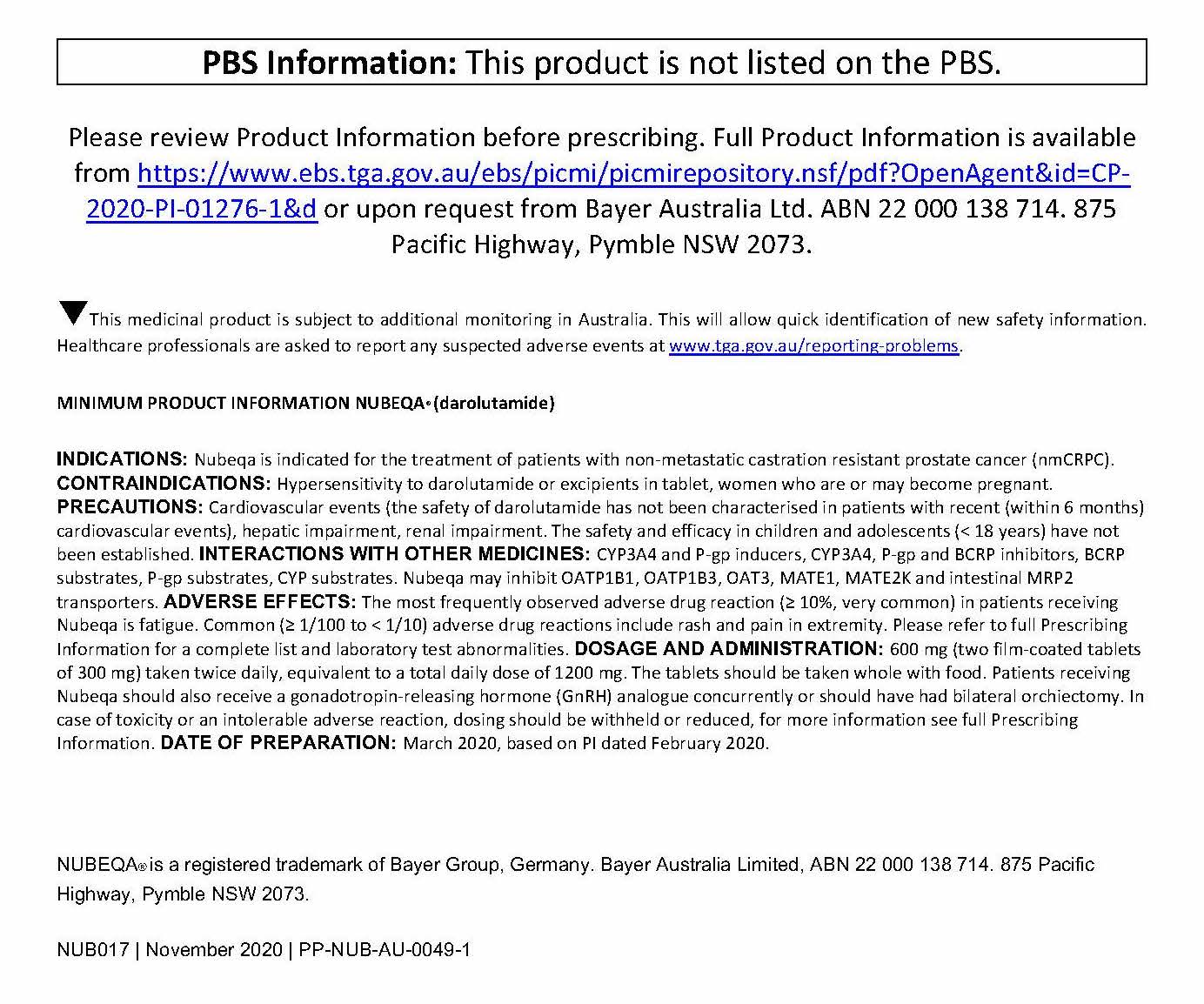
ARAMIS was a randomised, double-blind, placebo-controlled trial in men with nmCRPC and a prostate-specific antigen (PSA) doubling time of 10 months or less (n=1509). Patients received either darolutamide (600mg twice daily) or placebo while continuing ADT. The trial met its primary endpoint of metastases-free survival (MFS): the median MFS was 40.4 months with darolutamide plus ADT versus 18.4 months with placebo plus ADT (HR 0.41; 95% CI, 0.34 – 0.50; P<0.001). This benefit was consistent among patients with different baseline characteristics, therapies at baseline, and demographics.
The ARAMIS authors concluded, “…metastasis-free survival was significantly longer with darolutamide than with placebo for men with nonmetastatic, castration-resistant prostate cancer and a PSA doubling time of 10 months or less.” A stratified analysis found that darolutamide significantly improved MFS regardless of whether PSA doubling time at baseline was ≤6 months or >6 to ≤10 months, confirming the benefit in both groups of patients.
The final analysis of the study2 showed that darolutamide plus ADT also resulted in a statistically significant 31% reduction in the risk of death compared to placebo + ADT (HR 0.69; 95% CI, 0.53-0.88, P=0.003). This was considered by the panel to be in line with the results of studies with other ARis.5,6
Time to pain progression, time to cytotoxic chemotherapy, and time to a symptomatic skeletal event were also significantly improved with darolutamide plus ADT versus placebo plus ADT.2 Doctor Shore explained that these are all meaningful outcomes for patients, but noted that patients and clinicians often look at different aspects of treatment when weighing up the benefits and risks. “I’ve gotten much better at talking to patients about why I select therapies,” he said. “When I describe these findings to patients in my clinic, [I explain] it’s that we may see the PSA come down, which is always of keen interest to patients. As clinicians, we know it’s about time to progression and survival [benefits]…I describe this benefit to patients as being able to delay tumour burden – radiographic metastases – by almost 2 years,” he explained.
Tolerability profile of darolutamide
Doctor Shore explained that the distinct molecular structure of darolutamide and its low penetration of the blood-brain barrier results in a generally well tolerated safety profile.
The incidence of adverse events in the ARAMIS trial was similar for the darolutamide plus ADT and placebo plus ADT arms, 1,2 and the most common adverse events had a low incidence of Grade 3–4 events. The most frequently reported adverse event was fatigue.1,2 Doctor Shore noted that darolutamide was not associated with a higher incidence of seizures, falls, fractures, cognitive disorder, or hypertension compared to placebo.
Real-world experience with darolutamide
Webinar panellist Doctor Niara Oliveira from the Mater Hospital Brisbane presented a case study from her clinic to demonstrate real-world experience with darolutamide. Her patient was an 86-year-old man with nmCRPC after around two-and-a-half years’ ADT. He was referred to her department in January of this year with a PSA of 2.4. He declined radiotherapy to the prostate, and with no available PBS-subsidised treatment at the time, remained on ADT alone.
By July, the patient’s PSA had risen to 7.4 and by September it had risen to 8.7. At that point he started treatment with darolutamide and after four weeks’ treatment his PSA had declined to 2.5. He reported mild nausea upon commencement of therapy but no other concerns. He continues to do well, said Doctor Oliveira.
Doctor Shore presented a case study of a man in his early 70’s who responded well to treatment. While his case illustrated treatment approaches with darolutamide in younger patients, he noted that Doctor Oliveira’s case study demonstrated the benefit of a well-tolerated treatment even in older patients with good performance status who have anxiety about their disease progression but expect to continue a good quality of life.
Optimising the decision-making process
The panel discussed how to best approach personalised treatment decisions. Doctor Shore listed his ‘four Ps’ of treatment goals that he discusses with patients: prolong survival, preserve quality of life, prevent complications of therapy, and preference value (the patient’s ‘risk-benefit’ profile).
The panel agreed that maintaining a good quality of life is an important treatment goal – particularly for long-term treatments that prolong life – and noted the negative impact of adverse effects such as fatigue and neurocognitive effects on quality of life. “We have not traditionally reflected well on our proactive recommendations on fatigue and daily lifestyle adherence…and certainly we haven’t done as good a job at establishing baseline cognition, depression and mood concerns,’ said Doctor Shore. Webinar panellist Professor Declan Murphy from the Peter MacCallum Cancer Centre in Melbourne agreed, noting that simple assessment tools and a multidisciplinary approach to assessment should be more widely used to monitor cognition.
The measurement of PSA doubling time was raised as an issue throughout the webinar discussion, and it was noted that it’s likely to become more important in the decision paradigm now with the availability of effective treatments for nmCRPC. It was suggested that clinicians will need to move from ‘back-of-the-envelope’ rough calculations to a more accurate measure of PSA doubling time using established calculators. The panellists agreed that this will help better identify patients who would benefit from treatment.
With a choice of therapies now available for patients with nmCRPC, the panel discussed their approach to their choice of upfront therapy. Doctor Oliveira said that she thought it was important to avoid reserving preferred treatments to later in the treatment sequence. “In older patients [in particular] you may only get one bite of the cherry, so I think it’s important to use your preferred treatment upfront – take your best shot at it,” she said.
References
- Fizazi K, et al. Darolutamide in nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2019;380:1235-1246. https://www.nejm.org/doi/full/10.1056/NEJMoa1815671
- Fizazi K, et al. Nonmetastatic, castration-resistant prostate cancer and survival with darolutamide. N Engl J Med. 2020; 383:1040-1049. https://www.nejm.org/doi/pdf/10.1056/NEJMoa2001342
- Smith M, et al. Apalutamide treatment and metastasis-free survival N Engl J Med. 2018;378:1408-1418. https://www.nejm.org/doi/full/10.1056/NEJMoa1715546
- Hussain M, et al. Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2018;378:2465-2474. https://www.nejm.org/doi/full/10.1056/nejmoa1800536
- Smith MR, et al. Apalutamide and overall survival in prostate cancer. Eur Urol. Published online September 6, 2020. https://doi.org/10.1016/j.eururo.2020.08.011
- Sternberg CN, et al. Enzalutamide and survival in nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2020;382(23):2197-2206. https://pubmed.ncbi.nlm.nih.gov/32469184/