Delays in surgery for cancer due to COVID-19 pandemic disruption will have a significant impact on patient survival, a new UK study shows.
While surgery is being prioritised for aggressive cancers during the COVID-19 pandemic, delays of as little as three months for cancers with a favourable prognosis will result in a significantly higher mortality burden for common cancers, a modelling study based on international data has found.
Delays in cancer surgery “will also result in tumours being more advanced, meaning not only that is survival poorer, but that the upstaged cancers will be more costly to treat both in terms of surgery and/or chemotherapy,” warn oncologists from the Institute of Cancer Research in London.
“Furthermore, resource requirements (for example, ICU stay) are dramatically higher for the many who will inevitably present as emergencies such as with obstruction, perforation or acute bleeding of the gastrointestinal tract,” they write in the Annals of Oncology.
And even in a setting such as the UK with high rates of COVID-19 disease, the excess cancer deaths resulting from delaying surgery by six months will approximate to 60% of the lives saved from treating COVID-19, they estimate.
In their study they modelled the impact of delays of three months and six months in cancer surgery on hazard ratios of cancer progression from observational 46 studies and applied these to age-specific, stage-specific cancer survival, in terms of lives saved and life-years gained.
As expected, they found that the greatest increases in mortality would arise following delays to surgery in aggressive cancers, with over 30% reduction in survival at six months and over 17% reduction in survival at three months for patients with stage 2 or 3 cancers of the bladder, lung, oesophagus, ovary, liver, pancreas and stomach.
But even modest delays of three or six months would have a significant increase in the number of excess deaths for early stage cancers such as for the bowel, lung or breast, particularly in younger people.
They estimated an overall reduction in life years gained from surgery of 1.0 years per patient with three months’ delay and 2.3 years with six months delay.
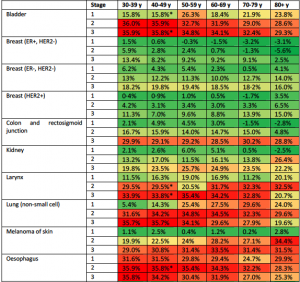
Reductions in five year survival with a six month delay in cancer surgery.
In their UK model, a delay of surgery by six months would result in 208,275 lost life years for an annual quota of surgical patients: which equates to 59% of the life years gained from hospitalisation of an equivalent number of community-acquired COVID-19 cases, after adjusting for resources.
“Delay in cancer surgery will have a highly deleterious health and economic impact. For the most part, the surgery will still be required (and may be more complex and costly) but results in rapid diminution resultant life-years gained and resource-adjusted life-years,” they wrote.
The researchers provided modelling of which cancer patients would be most affected by surgery delays and said this could be applicable internationally
“We propose a model that provides a rational approach by which to evaluate across patients of different ages, tumour types, and stages, the benefit and resource implications of their cancer surgery.
They said the model shows which groups of patients will be the most rationale to delay, and also provides information on those for whom backlogs in surgery would likely occur and where additional resources would need to be targeted.
“Supra-normal capacity is required to manage backlogs of accumulated cancer cases alongside ongoing incident cases. To avoid a deferred public health crisis of unnecessary cancer deaths, urgent ringfencing of substantial resources is required.