In a recent Amgen-sponsored Multiple Myeloma Expert Forum in July 2021, Dr Leo Rasche (attending physician on the myeloma service at the University Hospital of Würzburg, Germany) and Professor Gordon Cook (Clinical Director Haematology, Leeds Institute of Clinical Trials Research, University of Leeds, UK) gave their perspectives on delineating tumour heterogeneity in multiple myeloma (MM) and finding a cure for MM, respectively.
Understanding inter- and intra-patient tumour heterogeneity in MM with Dr Rasche
Dr Rasche’s presentation provided insight into the heterogenous nature of MM. He explained, “there are two types of heterogeneity: inter-patient variation, or variations of tumour features between patients; and intra-patient variation, or variation of tumour features within one tumour.” The benefit of understanding this concept is essential in the era of targeted immunotherapies, as residual disease may occur if the molecular subtypes differ within an individual,1 he said.
To better explain how different types of heterogeneity occur, Dr Rasche covered the pathophysiology of MM. “An initiating event such as a translocation or hyperdiploidy occurs in the lymph node, creating the first malignant plasma cell. This is then seeded in the bone marrow where they remain for ages, undergoing further evolution from additional drivers. These may include regional evolution, neo-angiogenesis, immune paralysis/escape and establishment of a permissive microenvironment,” he explained. “The initiating events are what leads to inter-patient heterogeneity, while the progression within an individual is what gives rise to intra-patient heterogeneity,” he said.
The importance of focal lesions
Dr Rasche explored the “poorly understood imaging phenomenon” of focal lesions in MM. He highlighted that MM is “both a solid and haematologic tumour” and noted their appearance upon imaging using the following methods:
- PET: Focal area with increased FDG-uptake in comparison to surrounding bone marrow
- DW-MRI: focal area with increased cellularity
- Histology: Plasma cell tumour
- FACS: Plasma cells and bystander/microenvironment cells
The work of Dr Rasche and his team found that “the mutation profile found in focal lesions can be different to that of the standard iliac crest biopsy – which can have an impact on prognosis.” The image below outlines how the pathogenesis of MM can lead to the development of focal lesions with a different molecular profile within a single patient.2 In it, you can see how the initial event occurs in the lymph node, is seeded in the bone marrow, leading to monoclonal gammopathy of undertermined significance (MGUS), before being replaced in a Darwinian ‘survival of the fittest’ fashion by cells that have mutated to better survive (clonal sweep). This leads to the MGUS being replaced with MM progenitors, when regional evolution and secondary driver events like those mentioned above cause localised mutations, seen as focal lesions under imaging.2
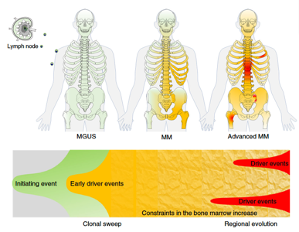
Image from: Rasche L, et al. Nat Commun 2017;8(1):268.
To summarise, Dr Rasche reiterated that MM is a heterogenous disease, and understanding the mechanisms of inter- and intra-patient heterogeneity as well as combining molecular tests with imaging technology can be important for predicting risk and when monitoring for residual disease in patients.1
Defining ‘cure’ in MM with Professor Cook
Professor Cook began his presentation with a brief overview of how far OS has come in MM patients since the ‘50s when melphalan came into play. He then compared various definitions of the word ‘cure’ – from the Oxford English Dictionary definition of “to relieve a person of the symptoms of a disease or eliminate a disease with medical treatment” to the difference between an ‘operational cure’ and a ‘statistical cure’. He suggested, “When we are thinking about cancer, we might want to think more about operational cure, which is where the patient actually has the disease controlled in such a way that they have a good quality of life, and succumb to something other than myeloma, like old age, while statistical cure can be defined as the adequate suppression of residual malignant cells to achieve sustained freedom from progression.” He gave examples of how these three definitions of cure apply to different cancers, with some cancers requiring treatment leading to cure (according to the Oxford definition), while others require treatment to reduce the tumour burden and allow long-term survival with good quality of life (operational cure or statistical cure).
In MM, however, due to the clonal evolution and heterogeneity (described earlier by Dr Rasche), treatment needs to adapt to disease emergence and clonal variation.
Factors in long-term survival
In order to answer the question ‘Is it timely to discuss a cure?’ Professor Cook took his audience through data from long-term trials. However, he reminded the audience that this necessarily meant looking at trials using older treatment protocols to what are used in the modern era of MM therapy. “In order to get robust long-term data then you’re going to need to look at patients treated in a different era to what we are used to these days. Most treatments will be without novel therapies, so bear that in mind,” he explained.
When looking at comparisons of predicted remaining lifespan vs actual lifespan of patients with MM, the number of patients meeting their predicted lifespan is “remarkably similar throughout the years: approximately 15%,”3 said Prof Cook. He highlighted factors that seem to contribute to long-term survivorship:4
| Increased chances of long-term survivorship | Reduces chances of long-term survivorship |
| Sustained response* | Age |
| Novel agent based inductions | Tumour burden |
| Tandem ASCT | Poor organ function |
| Maintenance therapy* |
*Significantly improves chances of long-term survivorship.
In addition to these factors, kinetics of disease control (MRD-negative status, achieving complete response) and make-up of the immune system (presence of senescence) “may well be linked to long-term survivorship,” explained Prof Cook.
How to pursue a ‘cure’
Prof Cook turned to the variety of therapeutic agents now in use, including immunotherapies. He presented data showing “we have therapeutic technologies that can drive deeper responses. Therapeutic options are only increasing as we go through time, and this is important because with new therapy the 5-year relative survival rate has improved.” He concluded by saying, “Where we’re going with immunotherapeutic strategies remains to be seen, but the 5-year survivorship rate is only likely to improve”.
| Take-home messages
Dr Rasche’s work highlights the need to further understand inter- and intra-patient heterogeneity in order to overcome intra-patient variations before a cure can be truly found for MM.1 Speaking of a cure, Professor Cook recommended considering “less about life years gained, and more about life years lost, which pays homage to the concept of operational cure”. |
[Footnotes]
ASCT=autologous stem cell transplant; DW-MRI=diffusion-weight magnetic resonance imaging; FACS=fluorescence-activated cell sorting; FDG=fluorodeoxyglucose; OS=overall survival; PET=positron emission tomography.
References:
- Rasche L, et al. Int J Mol Sci 2019;20(5):1248.
- Rasche L, et al. Nat Commun 2017;8(1):268.
- Nishimura KK, et al. Blood Adv 2020;4(2):422-431.
- Lehners N, et al. Cancer Med 2018;7(2):307-316.
- Shah UA and Mailankody S, BMJ 2020;370:m3176.