Clinicians need to take time out to consider other approaches to the long-term management of primary immune thrombocytopenia (ITP) in patients not adequately responding to first-line therapy, according to haematologist Danny Hsu from the Liverpool hospital in New South Wales. “For patients without a sustained and consistent response on first-line therapy, it’s important to take a step back and consider whether it’s time to choose an alternative therapy,” he says. “The next step is to find the best second-line option, and perhaps consider whether your patient is appropriate for thrombopoietin receptor agonists (TPO-RAs) by assessing their risks and comorbidities,” he explains.
The introduction of thrombopoietin receptor agonists (TPO RAs) and rituximab for ITP has broadened second-line treatment options beyond splenectomy,1 and have been endorsed by The International Consensus group on ITP as alternatives to splenectomy after first-line therapies have failed.2 Recent Chinese and Austro-German-Swiss guidelines have also endorsed the use of TPO RAs as second-line agents, before consideration of splenectomy.3,4
Splenectomy offers the highest cure rate of all therapies for adult ITP, with a long-term response of 60–70% at five to ten years.1 However, its use has declined over recent times, often being restricted to younger patients because of the higher risk of surgical complications in patients over 65 years of age, and also the lower response rates.1 “Splenectomy may be a suboptimal therapy in older patients,” says Dr Hsu. “It’s most effective in patients aged less than 40 years old where some studies have shown that this age group has the highest chance of platelet response or clinical cure,” he explains.
There is also a growing understanding of the consequences of spleen removal. “We are starting to appreciate the long-term effects of splenectomy, including thrombotic risk and ongoing risk of sepsis,” Dr Hsu says. “Patients are acutely aware that splenectomy is a one-way street: you can’t reverse it,” he adds.
Patient preference may also be a factor in the decline in splenectomy rates, with patients increasingly aware of other second-line alternatives.1 “Some patients simply won’t consent to having their spleen removed,” says Dr Hsu.
Eltrombopag efficacy in adult ITP
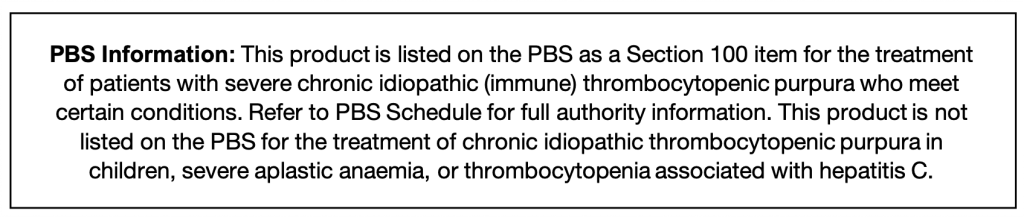
Eltrombopag (Revolade®) is an orally-administered TPO-RA indicated for second-line treatment for adults with chronic ITP who have had an inadequate response or are intolerant to corticosteroids and immunoglobulins.5 It has been shown to be effective regardless of splenectomy status.6 It is listed as a PBS authority item for patients who have failed to achieve an adequate response or are intolerant to corticosteroid and immunoglobulin therapy, and have had a splenectomy or are unsuitable for splenectomy due to medical reasons.7
The long-term open-label EXTEND study in 302 patients who had a median duration of eltrombopag treatment of 2.37 years6 found that the therapy rapidly increased median platelet counts to ≥50 x 109/L by week 2 and maintained counts over two or more years.
Overall, 259 patients (85.8%) achieved the primary outcome measure of response (a platelet count of ≥50 x 109/L at least once in the absence of rescue), and 133 of 257 (52%) achieved a continuous response over 25 weeks or longer.6
Response rates were lower in patients who had received a high number of previous therapies, had undergone splenectomy, were receiving other ITP therapies at baseline, or had lower platelets at baseline. However, the authors note, “None of the differences between subgroups were substantial enough to be considered prognostic factors or to recommend using or withholding eltrombopag in specific patient subgroups.”6
Bleeding symptoms decreased from 57% at baseline to 16% at one year after treatment commenced. Rates of bleeding were found to decline in both patients who had had a splenectomy and those who had not, and most bleeding events during the study were WHO grade 1 or 2.6
Eltrombopag long-term safety data
Eltrombopag has been available in Australia since 2010.5 Doctor Hsu says that initial concerns of the potential for specific adverse events with TPO-RAs have been addressed with further clinical experience and also with published long-term data.6 “There were initial questions surrounding the risk of myelofibrosis, cataracts and liver function abnormalities with eltrombopag. My clinical experience and the long-term clinical data have shown that these issues are manageable,” he explains.
Long-term data includes the EXTEND study6 where there was a median duration of treatment of 2.37 years (2 days to 8.76 years). A total of 18 patients had been treated with eltrombopag for six or more years. Adverse events occurring in more than one patient in the cohort included hepatobiliary adverse events (n=7), cataracts (n=4), deep vein thrombosis (n=3), cerebral infarction (n=2), headache (n=2), and myelofibrosis (n=2). The authors report, “Rates of thromboembolic events (6%) and hepatobiliary adverse events (15%) did not increase with treatment duration past 1 year.”
The approved product information recommends regular monitoring of full blood counts and liver function throughout treatment.5 Dose adjustment for liver function abnormalities and thrombosis/embolism is also recommended.5
Real world data shows differences between second-line treatments
Recently published real world data has provided further insight into the relative efficacy and safety of second-line therapies for ITP. A large retrospective study (n=2047) analysed US electronic health record data of adults with chronic ITP who received second-line therapy after previous treatment with corticosteroids or immunoglobulins.8
The study compared platelet response and incidence of both bleeding-related episodes and thrombotic events over 12 months after initiating second-line therapies, which included eltrombopag (5.4%), romiplostim (9.2%), rituximab (72.7%), and splenectomy (12.7%). The mean age of patients was 60.8 years.8
Splenectomy was found to result in the highest mean platelet counts, in line with previous data showing the greatest response rates with this option.1 There were no statistically significant differences among the second-line treatments in thrombotic events. However, bleeding-related events were significantly lower with eltrombopag than with other treatments, ranging from 25.5% for eltrombopag to 36.5% for romiplostim (p=0.038).8
Patient acceptance of eltrombopag
Eltrombopag is administered as a once-daily tablet,5 which Dr Hsu believes is a particular advantage for many patients. “The alternative TPO-RA therapy is a subcutaneous injection. Unless the patient is happy to come into the hospital every week for the injection, they need to self-administer at home. This can be difficult for older patients who can find it hard to reconstitute the drug and draw up small volumes,” he explains. He notes that patients must remember to avoid taking the tablets at the same time as antacids, dairy products and mineral supplements. They also need to take the tablet at the same time each day in relation to food intake.5 “If they are mindful of the dietary considerations, the dose is timed properly and is taken as part of a daily routine, most patients find it quite manageable,” he says.
SEE APPROVED PRODUCT INFORMATION BEFORE PRESCRIBING. APPROVED PRODUCT INFORMATION IS AVAILABLE ON LINE AT EITHER HTTPS://WWW.NOVARTIS.COM.AU/PRODUCTS/HEALTHCARE-PROFESSIONALS/PRODUCTS OR WWW.EBS.TGA.GOV.AU/
References
- Ghanima W et al. How I treat immune thrombocytopenia: the choice between splenectomy or a medical therapy as a second-line treatment. Blood 2012; 120(5): 960–969 http://www.bloodjournal.org/content/120/5/960?sso-checked=true
- Provan D et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood 2010;115(2):168–186. http://www.bloodjournal.org/content/115/2/168
- Liu XG et al. Chinese guidelines for treatment of adult primary immune thrombocytopenia. IJH 2018;107:615–623 https://www.ncbi.nlm.nih.gov/pubmed/29619624
- Matzdorff A et al. Immune thromobocytopenia – Current diagnostics and therapy: Recommendations of a joint working group of DGHO, OGHO, SGH, GPOH, and DGTI. Oncol Res Treat 2018;41(suppl 5):1–30. https://www.ncbi.nlm.nih.gov/pubmed/30235458
- Revolade Approved Product Information https://www.novartis.com.au/products/healthcare-professionals/products
- Wong R et al. Safety and efficacy of long-term treatment of chronic/persistent ITP with eltrombopag: final results of the EXTEND study.
- Pharmaceutical Benefits Scheme. Eltrombopag listing https://www.pbs.gov.au/medicine/item/5825N-5827Q
- Said Q et al. Bleeding related episodes, thrombotic events and platelet counts among immune thrombocytopenia patients receiving second line therapy. Blood 2018;132:2436 http://www.bloodjournal.org/content/132/Suppl_1/2436
AU-10576 October 2019.