 A consensus document on the diagnosis and management of thrombotic microangiopathy (TMA) in Australia and New Zealand has highlighted the importance of treating patients empirically while waiting for ADAMTS13 test results.
A consensus document on the diagnosis and management of thrombotic microangiopathy (TMA) in Australia and New Zealand has highlighted the importance of treating patients empirically while waiting for ADAMTS13 test results.
Co-author Dr Tom Barbour told the limbic plasma exchange should be implemented early, especially in adults, given the potential for rapid progression to end-state organ failure.
“ADAMTS13 testing in all patients will differentiate thrombocytopenic purpura (TTP) from conditions that are not TTP. While testing is widely available, the time to get the results is variable,” he said.
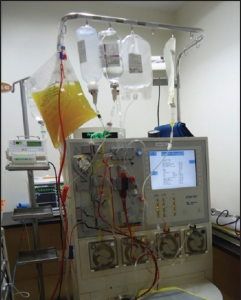
“Start plasma exchange and keep the patient safe while you wait for the test to come back to guide further treatment.”
The paper also said peripheral blood examination specifically looking for red cell fragments should be requested for any patients with thrombocytopenia and anaemia.
Dr Barbour, a nephrologist from the Royal Melbourne Hospital, said the consensus document was developed to help overcome a knowledge and practice gap.
“Some patients are referred to nephrology, some to haematology, and no one specialty is seeing all of the patients. We feel we all have an interest but are siloed in our own specialties.”
“And that has resulted in the need for engagement between specialties and liaison with other colleagues, for example in intensive care or obstetrics.”
The consensus document highlighted the potential for more than one aetiological factor to be involved in patients with TMA.
“We think when patients develop TMA, in many cases there is more than one reason. For example, a patient with a genetic complement problem and atypical haemolytic uraemic syndrome (aHUS) may then get an upper respiratory tract infection and is diagnosed with TMA.”
“A pregnant woman could also have a complement problem. The important thing is to keep an open mind. You can’t assume,” he said.
The paper reviewed the evidence for current pharmacotherapies such as eculizumab for aHUS and steroids for acquired TTP.
It also flagged novel therapies on the horizon such as caplacizumab for TTP.
“We envisage a time when additional monoclonal antibody therapies and other small molecules will be available for the treatment of these conditions,” Dr Barbour said.