The next edition of Australia’s Clinical Practice Guidelines for multiple myeloma (MM), due for release in early 2017, will highlight the dramatic changes to the treatment landscape in recent years that have resulted in positive steps towards progression free and overall survival for patients with multiple myeloma.
“In just three years since the release of the second edition in 2014, there will have been upfront approval for lenalidomide, there will likely be more concrete positive data on carfilzomib and daratumumab, and we will likely be nearer PBS approval for combination therapies in Australia,” said Professor Miles Prince, Director of the Centre for Blood Cell Therapies at the Peter MacCallum Cancer Centre. In this timeframe there has also been approval for pomalidomide in refractory disease.
“Three big advances have been the development of monoclonal antibodies, second-generation proteasome inhibitors, and much better insights into the mechanisms of disease,” said Professor Prince who is also chair of the medical and scientific advisory group producing the clinical practice guidelines.
“Treatment of refractory patients remains an unmet need, and in Australia we are stuck with a lack of combination therapies. There are some combinations that are clearly highly effective, so we are crossing our fingers that these will be allowed in Australia.”
While high-dose melphalan and autologous stem cell transplantation (ASCT) remain a cornerstone of therapy, a rapidly expanding array of new treatments for multiple myeloma means therapy has changed beyond recognition in the last decade.
Studies show that where haematologists previously expected the first remission to last between 9-12 months, 18 months to three years is now the norm – and this could push out to three to five years with the combination therapies showing promise internationally.
In this in-depth feature we speak to the experts to give you the latest on the newer agents responsible for changing the treatment landscape for the better.
Immunomodulators (IMiDs)
Thalidomide was the first IMiD used for patients with MM and until recently remained widely used to treat patients with relapsed MM. A phase III study, IFM 99-06, demonstrated a survival advantage when thalidomide was used in combination with melphalan and prednisone (MPT) compared to MP in the treatment of newly diagnosed multiple myeloma patients.
A derivative of thalidomide, lenalidomide was developed by what was then a small biopharmaceutical company called Celgene. The aim of the therapy was to improve efficacy whilst minimising some of the toxicity associated with thalidomide, such as peripheral neuropathy.
It was first approved in the United States in 2006 for use in combination with dexamethasone in MM patients who had received at least one prior therapy, and approval was expanded by the FDA and the European Medicines Agency in 2015 for newly-diagnosed patients. It was first approved for relapsed and refractory use in Australia in November 2009 and has now become a mainstay of multiple myeloma treatment in this country. A first line listing for lenalidomide has now been approved by the TGA and Celgene are currently pursuing PBS reimbursement..
“This arrival of lenalidomide is a huge advance because we have been stuck with thalidomide and chemotherapy, which just isn’t as well tolerated. Now we will have a drug that is well tolerated, maintains quality of life and gives prolonged remissions, which I think will be huge for multiple myeloma,” Professor Prince said.
Another derivative of thalidomide, pomalidomide was approved in Europe and the USA in 2013 for use with low-dose dexamethasone in patients with relapsed and refractory MM who have disease progression following at least two prior therapies, including lenalidomide and bortezomib. It was listed on the PBS in 2015 for patients with relapsed and refractory multiple myeloma who have failed lenalidomide and bortezomib. Like lenalidomide, its main side effects are haematological toxicities, though neuropathic toxicity and venous thromboembolic complications are low.
| Celgene: On a mission to make myeloma a chronic diseaseThe availability of immunomodulators in Australia is largely due to Celgene, which recently marked 10 years of myeloma research and development in this country.
The company has been responsible for bringing thalidomide, lenalidomide and pomalidomide to Australia and has invested heavily in improving the treatment of myeloma through investigator initiated and company sponsored clinical trials. Celgene also continues to invest in the education of physicians, a commitment illustrated by the fact that the company has been the platinum sponsor for the HSANZ / HAA annual conference for the past 9 years. Ultimately, Celegene’s vision is to help make myeloma a chronic disease. |
Proteasome inhibitors
Proteasome inhibitors have become an integral part of MM therapy, but can be challenging for patients because they require an infusion or a subcutaneous injection, while toxicity remains an issue. Bortezomib is listed on the PBS and is widely used for MM, however research interest is focusing on development of an oral agent, especially if it could be combined with an IMiD, to increase efficacy.
Carfilzomib is a second-generation proteasome inhibitor approved in the United States but only available in Australia currently through compassionate access schemes.
However according to Professor Prince it holds great promise because it is well tolerated with no evidence of neurotoxicity.
Ixazomib is the first oral proteasome inhibitor in clinical trials and has been granted orphan drug designation in multiple myeloma in the United States and Europe in. Meanwhile, research into newer proteasome inhibitors is making progress, with marizomib, oprozomib and VLX1570 in particular showing early promise.
Monoclonal antibodies (mAB)
According to Professor Prince a major advance in the treatment of MM has been the development of monoclonal antibodies.
“We have had success with these for lymphoma for a long time and have been looking in myeloma, but the problem is the off target effects of some of the antibodies have been substantial. Now we have two, with a third to follow, and that’s been a major addition to the armatorium,” said Professor Prince.
Elotuzumab, daratumumab and SAR650984 are all in development for the treatment of MM and appear to be well-tolerated and promising both as single agents and in combination with lenalidomide.
Following FDA approval in November 2015, the European Commission has this month approved elotuzumab in combination with lenalidomide and dexamethasone for patients with MM following progression on at least one prior therapy, based on the findings of a Phase III trial, ELOQUENT-2.
Another monoclonal antibody, daratumumab, has shown promise in Phase I and II studies. First designated a breakthrough therapy for MM by the FDA in 2013, it was granted accelerated approval in November 2015 as a monotherapy for patients with MM following at least three prior therapies.
In May 2016 it was granted conditional marketing approval by the European Commission for the treatment of patients with relapsed/refractory multiple myeloma who have been previously treated with a proteasome inhibitor and an IMiD and who progressed on their last therapy. Both approvals are awaiting results of confirmatory trials.
Combination therapies
Historically, combination therapies have proved disappointing in MM compared to standard melphalan and prednisone, with no greater efficacy and high rates of toxicity. However, the availability of the newer drugs, and their different mechanisms and better toxicity profiles, have led to mounting excitement over the possibility of combination therapies involving monoclonal antibodies, immune modulators and proteasome inhibitors.
However, according to Professor Prince a lack of PBS approvals for combinations of some of the novel agents remains a significant barrier to the progression free survival of patients in Australia.
Targeted therapies will offer new directions
Associate Professor Simon Harrison, the lead haematologist for myeloma at the Peter MacCallum Cancer Centre, said advances in understanding of the molecular basis of myeloma could continue to lead to better targeted therapies and more accurate treatment decisions.
He said the aim was to make myeloma a chronic disease: “The problem is that multiple myeloma is a constellation of a lot of different diseases that affect plasma cells, but as we understand more about the molecular basis it will become four to half a dozen molecular diseases.
Dividing it into molecular sub groups will help to inform treatment decisions and develop targeted therapies – we are probably treating more than one disease,” he said.
The significant problem of treatment refractory disease would also be answered with molecular testing, which would help to identify resistant clones and better target therapies.
He said combination therapies would also likely be central to improve response and duration of response at all stages of disease.
Antibodies are one of the most exciting areas of research, which had transformed the treatment of lymphoma and could do the same with myeloma. Centres around the world were trying to develop other immune-based cellular therapies to be even more effective, he said.
Specifically, check point inhibitors such as CTLA-4, PD-L1, or PD- , which were being looked at for many diseases, could hold great potential in myeloma.
“Myeloma is very immune suppressive. The development of new antibodies, cell-based therapies which turn on or re-engineer the immune system, and checkpoint inhibitors offer the most exciting strategies moving forward,” he said.
Myeloma Australia CEO Steve Roach said the organisation was working with pharmaceutical companies to advocate for combination therapy in Australia. However, he noted that nothing could be done formally until the submission was made to the PBAC.
“When it’s time to make submissions, it would be great for haematologists to say their piece and support these applications,” he said.
“[Combination therapy] could offer better life expectancy, better living conditions, they would keep people in the workforce, provide more treatment options and enable people to lead a more productive life.”
This article was sponsored by Celgene Pty Ltd Melbourne, which has no control over editorial content. The content is entirely independent and based on published studies and experts’ opinions, the views expressed are not necessarily those of Celgene Pty Ltd.
Before prescribing REVLIMID® (lenalidomide) please review the Product Information which is available at 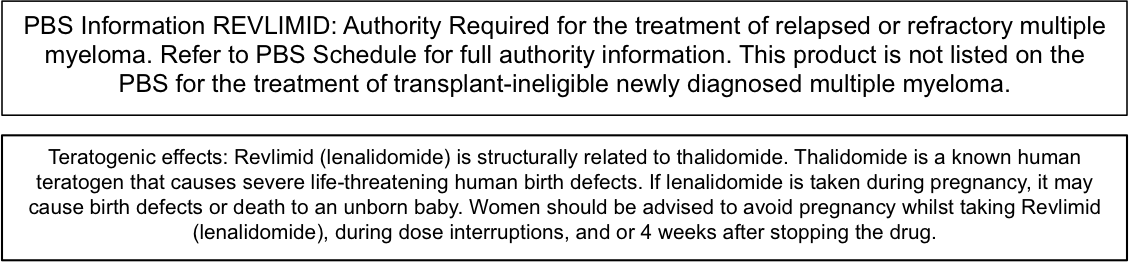
Before prescribing Pomalyst® (pomalidomide) please refer to the Product Information which is available at 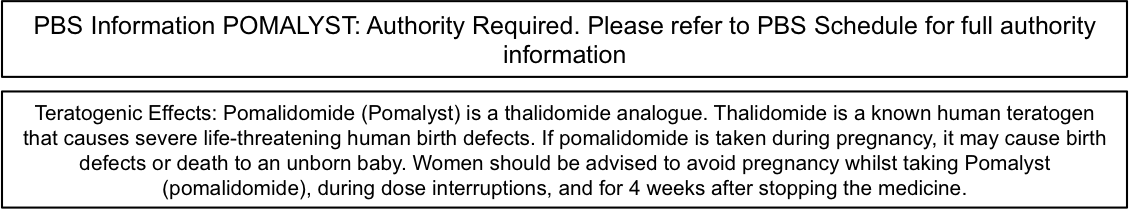
Before prescribing Thalomid® (thalidomide) please refer to full Product Information which is available at 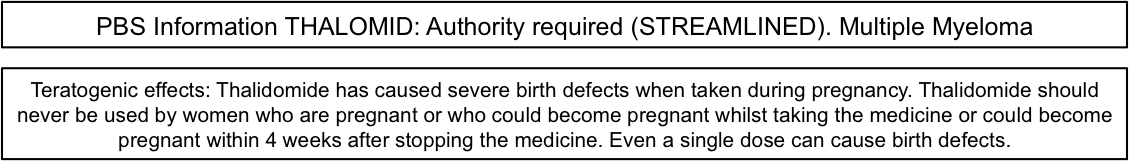
Further information is available from Celgene. Celgene Pty Ltd ABN 42 118 998 771. Level 15, 60 City Rd, Southbank, VIC 3006, Australia. Tel 1800 CELGENE (1800 235 4363) www.celgene.com.au ®Registered Trademark Date prepared: 10/2016.