On the 1 February 2017, Australia joined the US and Europe in making continuous therapy with Revlimid (lenalidomide) plus dexamethasone reimbursed on the Pharmaceutical Benefits Scheme for newly diagnosed transplant ineligible patients with multiple myeloma1. This is exciting news, and the limbic spoke with Dr Hang Quach, Consultant Haematologist at St Vincent’s Hospital, Melbourne, and member of the Australian Medical Scientific Advisory Group for Myeloma (MSAG), to gain insight into how this development will impact the way multiple myeloma is managed in Australia.
Approval of continuous therapy is a big deal
According to Dr Quach there are several reasons why the approval of lenalidomide/dexamethasone continuous therapy is a big deal. “Multiple myeloma remains an incurable disease, so with treatment we’re aiming to achieve a deep response, and we want to maintain that response for as long as possible – this is where continuous therapy comes in” she tells the limbic in an interview.
Continuous therapy also has the capacity to extend progression-free survival (PFS) and even overall survival (OS ) when compared to some fixed-duration approaches.
However, she notes that this cannot be at the expense of treatment toxicity, which may negate any survival benefit if a patient’s quality of life is severely impacted.
“That’s what has prevented continuous therapy from being the standard of care – until now,” 2 says Dr Quach, who is also the lead author of the current Australian guideline for the treatment of Multiple Myeloma for physicians.
Times are changing
The concept and research into continuous therapy in multiple myeloma itself has been around for over 30 years, however, long-term continuous use of treatments were met with limited success due to the cumulative toxicity of agents such as thalidomide, interferon and corticosteroids.3 This is why thalidomide, which has until recent been the only agent available for “maintenance“ therapy on the Pharmaceutical Benefits Scheme (PBS), can only be given for an average of only 12 months, primarily due to neuropathic toxicity associated with longer-term treatment.2
However, continuous therapy may be set to make a revival with a subset of frontline patients. The recent approval of continuous therapy with lenalidomide makes it now an option for transplant-ineligible patients.1 Furthermore, ever more intensive research continues into other agents including next-generation proteasome inhibitors, monoclonal antibodies, histone deacetylase inhibitors, and more.3
It took years to get to where we are today
Continuous therapy is a well-accepted standard of care in many countries across the world for both young, transplant eligible and older transplant ineligible patients. “However despite the emerging clinical trial evidence, there remains a school of thought that the goal of therapy in multiple myeloma is to get patients off therapy,” Dr Quach explains. “However, as multiple myeloma remains an incurable disease, continuous therapy is about maintaining a durable response to treatment for as long as possible, when the treatment is tolerated by the patient.”
For patients who are not eligible for autologous stem cell transplantation (ASCT), the standard treatment until now typically consisted of a chemotherapy agent (typically cyclophosphamide or melphalan) and prednisone plus either bortezomib or thalidomide for a given number of fixed cycles.4
However the results from the large Phase three study, Frontline Investigation of Revlimid and Dexamethasone versus Standard Thalidomide (FIRST) has demonstrated the significant benefit of continuous lenalidomide and may represent a shift away from fixed-duration treatment to continuous therapy.5
The results of the trial, which examined continuous versus fixed-duration treatment demonstrated a longer time to progression-free survival compared with melphalan/prednisone/thalidomide or fixed-duration treatment with lenalidomide/dexamethasone.5
The final analysis of this study with longer-term follow up has now confirmed the OS benefit in favour of the continuous lenalidomide/dexamethasone arm, compared to melphalan/prednisone/thalidomide, which until now has been one of the accepted standards of care.6
Dr Quach says trials like these give clinicians confidence in treating patients, “What this and other trials give us as clinicians is Level 1B evidence (ie. strong evidence based on large randomised clinical studies) around the use of continuous therapy in patients not eligible for ASCT.”
“What the results from the FIRST and other continuous therapy studies has also given us is new heights (or rather lows) in depth of response and durability of that response”, says Dr Quach. There is now evidence that a deeper, durable response to treatment translates to better survival long term.7
How long is long enough when it comes to continuous therapy?
While the data is very favourable in terms of continuous therapy, there have been some questions raised by clinicians about how long is long enough, should continuous therapy be offered to every patient and whether there are risks that need to be considered?8,9 Dr Quach explains, “Yes, we know there are a small number of patients who will still do well without maintenance therapy after their initial treatment, however, there are currently no biomarkers to screen for these patients, so we have to assume everyone needs it at this point in time.”
“In using lenalidomide and dexamethasone as upfront treatment for transplant ineligible patients, treatment should be continued until disease progression and the only factor that should impact on the physician’s decision to ‘cap’ continuous lenalidomide therapy is if the patient develops unacceptable side effects, “ she adds.
So, is it the time patients have been waiting for?
Perhaps for some, but as Dr Quach points out, it’s still going to be a very individual journey for each patient. In the end, it will come down to individual patient tolerability, says Dr Quach who notes that, “most of my patients would rather live well than live longer on an intolerable treatment.”
“It’s really thanks to the research of our predecessors in multiple myeloma that we have better options for patients now and hope for the future. It offers them yet another step towards living longer, with the quality of life they hope for.”
This article was sponsored by Celgene Pty Ltd Melbourne, which has no control over editorial content. The content is entirely independent and based on published studies and experts’ opinions, the views expressed are not necessarily those of Celgene Pty Ltd.
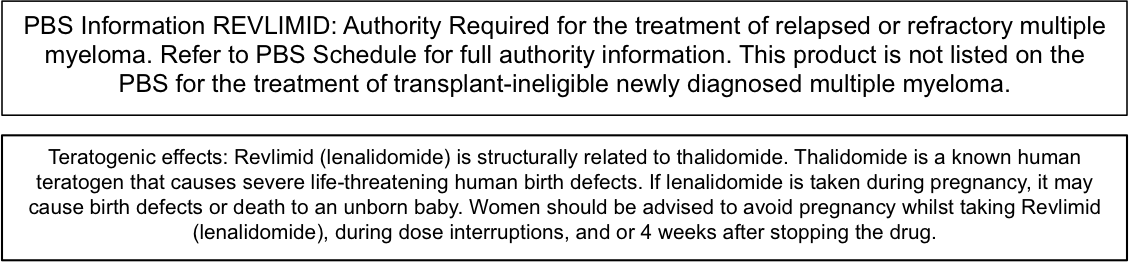
Before prescribing REVLIMID® (lenalidomide) please review the Product Information which is available at http://www.guildlink.com.au/gc/ws/celgene/pi.cfm?product=cjprevli
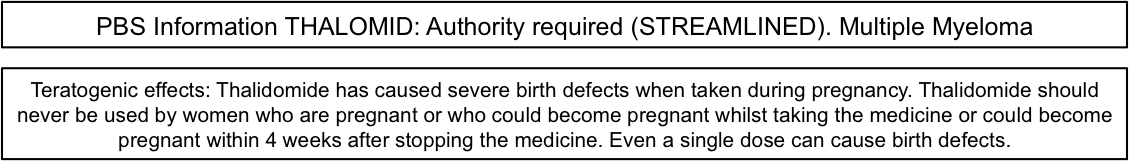
Before prescribing Thalomid® (thalidomide) please refer to full Product Information which is available at http://www.guildlink.com.au/gc/ws/celgene/pi.cfm?product=cjpthalo
References:
- Australian Government. Department of Health. Pharmaceutical Benefits Scheme, Available from: http://www.pbs.gov.au/ (accessed 14 Feb 2017).
- Facon T Hematology Am Soc Hematol Educ Program 2015;2015:279–85.
- Lipe B et al. Blood Cancer J 2016;6(10):e485.
- Medical scientific advisory group (MSAG) to the Myeloma Foundation of Australia (MFA). Clinical practice guideline multiple myeloma, 2015.
- Benboubker L et al. N Engl J Med 2014;371(10):906–17.
- Facon T et al. Blood 2016;128(22):241.
- Rawstron AC et al. Blood 2015;125(12):1932–5.
- Palumbo A et al. J Clin Oncol 2015;33(30):3459–66.
- Wang Y et al. J Natl Cancer Inst 2016;108(3).