 An expert panel has made recommendations to strengthen assessment of potential new treatments for coeliac disease.
An expert panel has made recommendations to strengthen assessment of potential new treatments for coeliac disease.
With a confusing array of histology, serology, immunological markers and patient-reported outcomes being used in clinical trials of novel coeliac treatments, an international taskforce has investigated which are the most appropriate.
The Tampere recommendations acknowledge the increasing number of trials underway for alternatives to the gluten free diet.
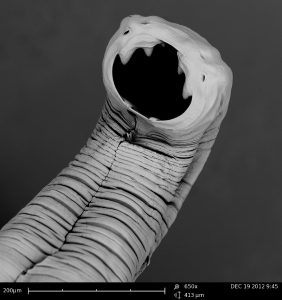
They include glutenases, gluten sequestrants, neutralising antibodies, lymphocyte blockers, tissue transglutaminase inhibitors, DQ2-blocking peptide analogues… and yes, hookworms.
Panel member Professor Marjorie Walker, co-director of the Priority Research Centre for Digestive Health and Neurogastroenterology at the University of Newcastle, told the limbic it was vital to establish robust outcome measures and stay ‘ahead of the game’.
“We don’t want to find a potential magic bullet for coeliac disease and not know how to measure if it’s any good or not.”
“What we’re looking at is the tests to see whether drugs that are not yet in general use are actually any good. So it’s terribly important to get it right because obviously there is a lot riding on it.”
“If you are a coeliac and on a gluten free diet it can be pretty unpleasant. And it would be nice if we had a treatment that meant even if you stuck to your diet but mistakenly took some gluten, you could actually say ‘That’s ok. I‘ll take this tablet and won’t feel sick’.”
The panel confirmed that histology was still the gold standard and an ‘essential outcome measure in any trials of coeliac disease treatment’.
Serology – IgA TG2 and IgG DGP – should also ‘at a minimum’ be measured at study entry and completion in coeliac disease treatment trials.
“Although cut-off ranges for diagnosis may not be optimal for monitoring response or predicting villous atrophy, any significant increase during a trial suggests increasing coeliac disease activity and may be used as a key outcome in some studies,” the panel said.
Although no immunological markers are yet been validated for therapeutic trials, they said a whole blood IFN-γ was a promising measure of immune responsiveness to gluten. At present immune markers should only be used as exploratory outcomes in phase ll and lll trials.
Gluten immunogenic peptides (GIPs) were also a promising tool in trials designed to prevent symptoms because of inadvertent gluten exposure.
Clinical end points in the form of patient-reported outcomes such as the Celiac Disease PRO (CeD-PRO) and the Celiac Disease Symptom Diary (CDSD) should also be included as a primary outcome in treatment trials.
They added that measurement of health-related quality of life should also be considered a critical end point ‘that may help to determine the overall value of a therapy or intervention to both patients and payors’.