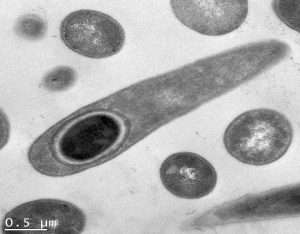
Sporulating C. difficile
Australian researchers have identified some potential strategies to prevent the cycle of Clostridioides difficile infection, transmission and recurrence.
The research team from Monash University have identified that cephamycins inhibit C. difficile spore formation – spores that spread and survive in the environment, challenge usual infection control practices and ultimately cause severe disease and mortality.
In their research published in Nature Microbiology, the team also found that cephamycins target the sporulation-specific penicillin-binding proteins (PBPs) in C. difficile.
Lead researcher Professor Dena Lyras, from microbiology department at Monash, said the findings offered two different strategies.
“The immediate use I can see for cephamycins is adding them to our standard of care to reduce sporulation within the patients and to reduce the chances of transmission and disease recurrence which happens in about 25% of patients when they are treated with, mostly, just vancomycin.”
The study found co-administration of vancomycin and cefotetan in infected experimental animals reduced recurrent disease compared to animals that received only vancomycin.
She told the limbic that having identified the molecular targets of cephamycins also opened up another course of action.
“In the end we have to move away from antibiotics and so now that we know the anti-sporulation target and we know what binds to that target, we can start working to find other alternative molecules that block that target but do not act as broad-acting antibiotics.”
She said if there was a C. difficile epidemic, cephamycins could be immediately added to the standard of care to prevent sporulation, transmission and disease recurrence.
“If you had to use it right now, you could.”
However there was more work to be done with optimising the drug to remain in the lumen of the gut and fine tuning its administration.
“A lot of these antibiotics were probably not formulated for this purpose and so there is work that needs to be done to look at how to dose, when to dose, how do put it together with the standard of care, etc.”
“Even more exciting, it doesn’t just work for C. difficile, it works for a bunch of other spore-forming bacteria.”
These included the food contaminant Bacillus cereus.
“Furthermore, our study provides evidence that targeting sporulation-specific PBPs may represent a viable route to anti-sporulation agents for other spore-forming bacteria that threaten human health, food safety and biosecurity,” the study concluded.