During his tour of Australia in 2018, Professor Joseph Verbalis, Professor of Medicine and Physiology, Chief of the Division of Endocrinology and Metabolism and Director of the Georgetown-Howard Universities Center for Clinical and Translational Science discussed the recent advances in the evaluation and treatment of hyponatraemia in the context of the condition’s long-standing history.
Hyponatraemia – or water intoxication – was first recognised nearly 100 years ago in the 1920s.1 Given the time of its discovery, the approach to its management is a textbook example of the foundations of translational science seen today. As Professor Verbalis explained, “translational science means translating basic science discoveries into clinical applications and clinical therapeutics. From the first animal model studies in 1926 that described water intoxication and the treatment of cerebral oedema with hypertonic saline solutions – it took about 11 years to translate that from animal studies into clinical use in 1938.”2
This approach to disease management is still highly relevant today, with some of the recent advancements in the understanding and management of hyponatraemia stemming from a translational scientific approach. Rather than just observation of symptoms on an individual patient level, today, as Professor Verbalis noted, “we are in the age of big data, meaning as opposed to a randomised controlled trial of a few hundred or thousand patients, we now have access through electronic medical records to hundreds of thousands – or even millions – of patients, and we can use the power of those number of patient records to discover relationships we did not know existed or to clarify them.” He demonstrated this through the relationship between hospital admission serum [Na+] and in-hospital mortality in over 53,000 patients published by Wald et al. 2010, which demonstrated a statistical inflection point at a serum [Na+] of 137 mEq/L – likely an asymptomatic patient, and much higher that most clinicians might clinically observe.3
“You shouldn’t ignore hyponatraemia, especially in younger patients – you need to look for a cause”
Professor Verbalis compelled Australian physicians to take hyponatraemia seriously. In this evolving field, studies continue to reveal adverse outcomes associated with hyponatraemia that warrant thorough investigation of its cause and effective management.
|
Cancer: Studies have shown a correlation between hyponatraemia and cancer. Of patients with cancer, those with co-morbid hyponatraemia had decreased survival and a recent study found that 13% of patients with hyponatraemia subsequently developed a diagnosis of head/neck or pulmonary cancer. Heart failure: A study has found hyponatraemia was also an independent predictor of mortality in hospitalised patients. Bone fractures and risk of falls: Studies have linked an increased risk of fracture in chronic kidney disease that is independent of osteoporosis and an increased risk of falls in patients with asymptomatic chronic hyponatraemia. |
Who should be treated in 2018?
Patients who are symptomatic should be treated, and the degree of symptomatology is a surrogate for the duration of hyponatraemia.10 When life-threatening symptoms present, it is usually acute and should be managed accordingly.10 When the patient is symptomatic, but less impaired it implies chronic hyponatraemia and you may have more time to consider how to treat the patient appropriately.10
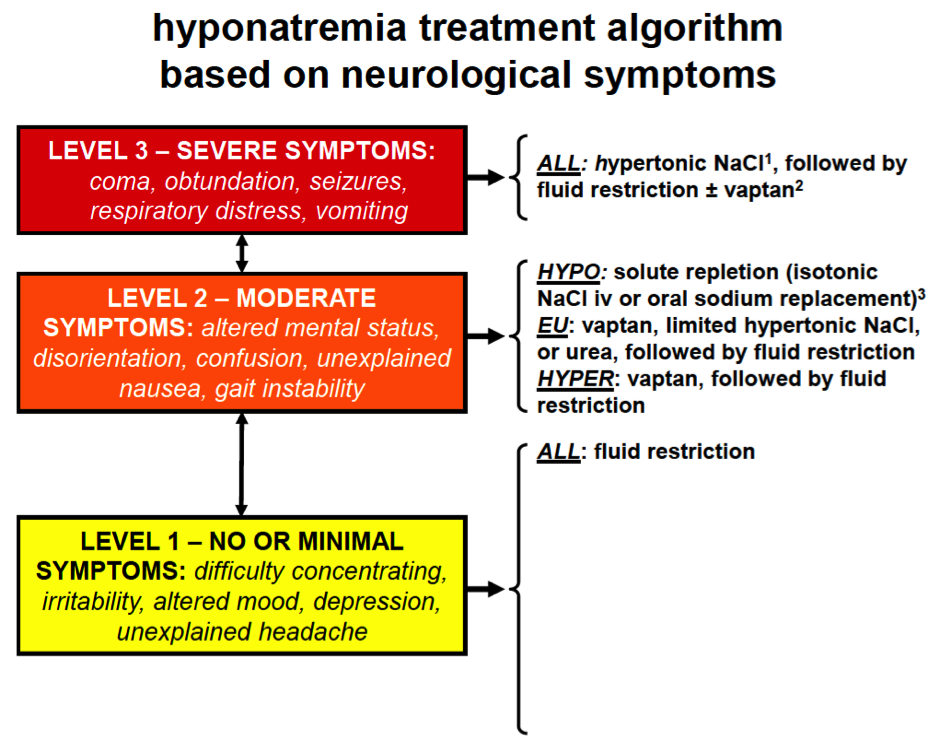
1some authors recommend simultaneous treatment with desmopressin to limit speed of correction.
2no active therapy should be started within 24 hrs of hypertonic saline to decrease the chance of overly rapid correction of [Na+] and risk of osmotic demyelination syndrome.
HYPO: hypovolaemic. EU: euvolaemic. HYPER: hypervolaemic.
Adapted from Verbalis et al. 2013.10
Finally, key to many treatments is fluid restriction, which Professor Verbalis says “you should be doing fluid restriction more intelligently than it is usually done. Predictors of failure of fluid restriction are less well known. These include:
- high urine osmolality (>500 mOsm/kg H2O
- when the sum of the urine Na+ and K+ concentrations exceed serum Na+
- when 24-hour urine volume is <1,500 mL/d
- when there is an increase in serum Na+ <2 mmol/L/d in 24-48 hours on a fluid restriction of ≤1 L/day. ”10
References
- Rowntree. Pharmacol Exp Ther 1926;29:135.
- Helwig et al. JAMA 1938;110:644.
- Wald et al. Arch Intern Med 2010;170:294-302.
- Doshi et al. Am J Kid Dis 2012;59:222-8.
- Schutz et al. Eur Urol 2014;65:723-30.
- Selmer et al. Eur J Intern Med 2016;36:36-43.
- Lee et al. JAMA 2003;290:2581-2587.
- Kinsella et al. Clin J Am Soc Nephrol 2010;5:275-280.
- Renneboog et al. Am J Med 2006;119:71.
- Verbalis et al. Am J Med 2013;126(10 Suppl 1):S1-42.