A recent sponsored educational meeting provided insights into the best-practice timeframe for initiating early intensive lipid-lowering therapy and its impact on the risk of major adverse cardiovascular events (MACE). It featured discussion by renowned Cardiologist Professor Shaun Goodman, Associate Head in the Division of Cardiology, Department of Medicine, at St. Michael’s Hospital and University of Toronto, Canada and A/Professor Karam Kostner, Director of Cardiology at Mater Public and Private Hospital Brisbane and Associate Professor of Medicine at the University of Queensland.
Prof Goodman presented the latest clinical evidence supporting strategies that lower LDL-C and reduce the risk of cardiovascular events in atherosclerotic cardiovascular disease (ASCVD). A/Prof Kostner shared his expertise from an Australian perspective, including a case study from his clinical practice.
High-intensity statins plus ezetimibe may not sufficiently lower LDL-C in some patients
Prof. Goodman drew on lessons learned in the PROVE-IT1 and IMPROVE-IT2 studies, which highlighted a significant challenge and unmet need among ASCVD patients in relation to achieving target LDL-C levels set by the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) Guidelines.1-3
He also shared data from the ODYSSEY OUTCOMES study.4 Data from this study and related sub-studies5,6,7 showed that the benefit of PCSK9 inhibition was greatest in high-risk patients (prior CABG, diabetes, and polyvascular disease), who showed similar relative risk reductions in MACE, but greater absolute risk reductions when compared with the overall trial population.4I
In addition to the reduction in LDL-C levels, the ODYSSEY OUTCOMES trial found that post-ACS patients (n=18,924) with elevated LDL-C levels despite high-intensity or maximal tolerated dose of statins randomised to alirocumab demonstrated a lower risk of recurrent ischaemic cardiovascular events (death from coronary heart disease, nonfatal myocardial infarction, fatal or nonfatal ischemic stroke, or unstable angina requiring hospitalisation) compared to those randomised to placebo (9.5% in alirocumab group versus 11.1% in the placebo group; HR 0.85, 95% CI 0.78–0.93; p<0.001 over a median 2.8-year follow-up). To prevent one primary end-point event, 49 patients (95%; CI 28 to 164) would need to be treated for four years, based on a 4-year Kaplan-Meier estimate.4
A subgroup analysis of high-risk groups – including prior CABG, diabetes, and polyvascular disease – found that although the relative risk reduction afforded by the addition of alirocumab to high dose statins was consistent in each subgroup compared with the overall study population, the absolute risk reduction was greater in each.5,6,7
The intensity and duration of LDL-C lowering is correlated with reductions in cardiovascular events
Prof Goodman presented an analysis of 33 randomised controlled trials that showed the relationship between LDL-C reduction and the duration of therapy,8 commenting that the point of this treatment strategy is to “get the LDL-C low and to maintain that for a long time”. The analysis highlighted that the combination of LDL-C reduction and duration of therapy correlated with the reduction in cardiovascular events.8
Prof Goodman also described the association between cumulative LDL-C exposure and CV outcomes in patients with homozygous familial hypercholesterolemia (HoFH), heterozygous FH (HeFH) and patients without FH,9 reinforcing the benefit of early interventions to alter the trajectory of LDL burden in these patients.
Earlier lowering of LDL-C confers the greatest benefit to high-risk patients
Prof Goodman highlighted treatment gaps in current care strategies in post-ACS patients, both in Canada (Canadian VIGOUR Centre study)10 and in Australia (CONCORDANCE).11 In the Canadian registry-based study, the investigators found that around 80% of patients did not reach target LDL-C levels when tested at follow-up appointments 90 days later.10 In the Australian study, only 55% of post-ACS patients were treated with intensive lipid-lowering therapy 6–12 months after their hospitalisation.10
Data from the SWEDEHEART Registry showed the benefits of early lowering of LDL-C in post-myocardial infarction (MI) patients.12 The study found that an early LDL-C reduction and more intensive statin therapy after MI were associated with a reduced risk of MACE as well as reduced all-cause mortality.12
The need for additional lipid-lowering therapies in Australia
A/Prof Karam Kostner shared his perspective on the position of PCSK9 inhibitors in the Australian treatment landscape, referring again to the CONCORDANCE data, which indicated that up to 45% of Australian ASCVD patients were missing out on high-intensity lipid-lowering therapy in the 6 – 12 months after their ACS.11.
A/Prof Kostner illustrated the potential value of adding a PCSK9 inhibitor to lipid lowering therapy via a case study of a patient with multivessel disease and HeFH who had experienced ACS (NSTEMI). He demonstrated the Sanofi online interactive tool to help guide prescribers through the PBS eligibility criteria ahead of the PBS Authority application for alirocumab.
An online tool to help navigate PBS application for Praluent (alirocumab)
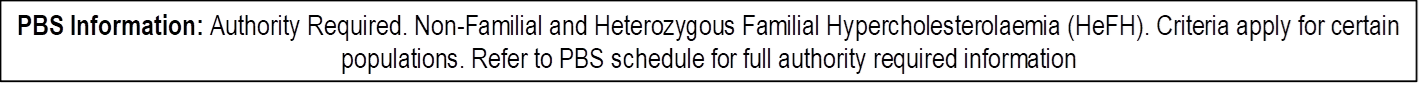
Praluent is an Authority Required PBS listed product13 for Non-Familial and Heterozygous Familial Hypercholesterolaemia (refer to PBS schedule for further criteria and restrictions). For demonstration purposes the talk focused on the Non-familial hypercholesterolemia patient depicted as:
- Symptomatic ASCVD, on diet and exercise
- Using maximum-tolerated statin + ezetimibe for >12 weeks
- LDL-C >2.6 mmol/L
- Additional CV risk factors (including severe multivessel CHD)
An online tool developed by Sanofi uses a simple 4-step process to assist prescribers in review of criteria ahead of the Authority application process:
- Select the PBS subsidy indication relevant to their patient.
- Enter the patient’s current lipid treatment.
- Add the patient’s LDL-C level (recorded within the last 8 weeks).
- Add other criteria (such as CV risk factor)
Training and support for patients
Sanofi has partnered with a team of pharmacists to offer patients injection training support. In addition, physicians are able to apply for a training device to instruct patients during consultations.
Disclaimers
Praluent® is indicated to reduce the risk of cardiovascular events (myocardial infarction, stroke, unstable angina requiring hospitalisation) in adults with established cardiovascular disease, in combination with optimally dosed statins and/or other lipid-lowering therapies.14
This article was commissioned by Sanofi Australia Pty Ltd. The content is independent and based on studies and the author’s opinion. The views expressed do not necessarily reflect the views of Sanofi. Before prescribing, please review the Praluent® (alirocumab) full product information 14 via the TGA website. Treatment decisions based on these data are the responsibility of the prescribing physician.
Please review full Product Information before prescribing. For full Product Information click here or contact Sanofi Medical Information on 1800 818 806.
MINIMUM PRODUCT INFORMATION: Praluent® (alirocumab (rch)) INDICATIONS Primary hypercholesterolaemia: as an adjunct to diet and exercise to reduce LDL-C in adults with primary (heterozygous familial or non-familial) hypercholesterolaemia in patients with moderate to very high cardiovascular risk: – In combination with a statin, or statin with other lipid-lowering therapies in patients unable to reach LDL-C goals with maximum tolerated dose of a statin, – alone or in combination with other lipid lowering therapies in patients who are statin intolerant or for whom a statin is contraindicated who are unable to reach LDL-C goals. Prevention of cardiovascular events: to reduce the risk of cardiovascular events (myocardial infarction, stroke, unstable angina requiring hospitalisation) in adults with established cardiovascular disease, in combination with optimally dosed statins and/or other lipid-lowering therapies (see full PI). DOSAGE AND ADMINISTRATION 75 mg subcutaneously every 2 weeks or 300 mg every 4 weeks. May increase to 150 mg every 2 weeks if inadequate LDL-C response. Measure lipid levels from 4-8 weeks of initiating/titrating Praluent, to assess response and adjust dose if needed. To administer 300 mg, give two 150 mg injections consecutively at two different injection sites. Inject into thigh or abdomen or upper arm that is not tender, bruised, red or hard (rotate site). Allow to warm at room temperature (up to 25°C) for 30-40 min before injecting; do not warm in any other way. See full PI. CONTRAINDICATIONS Hypersensitivity to the active substance or to any of the excipients. PRECAUTIONS General allergic reactions, immunogenicity, very low LDL-C levels (long-term effects unknown), pregnancy (category B1), lactation, children (< 30 mL/min/1.73 m2 ) not studied. INTERACTIONS Not anticipated. ADVERSE EFFECTS Common adverse reactions: injection site reactions, pruritus, upper respiratory tract signs and symptoms. Others, see full PI. NAME OF SPONSOR Sanofi-Aventis Australia Pty Ltd, 12-24 Talavera Road, Macquarie Park, NSW 2113. DATE OF PREPARATION 14 January 2020. Based on Full Product Information with TGA date of approval of 17 May 2016, with most recent amendment on 10 January 2020. Praluent® is a registered trademark of Sanofi-Aventis Australia Pty. Ltd trading as Sanofi, ABN 31 008 558 807 Talavera Corporate Centre, Building D, 12-24 Talavera Road, Macquarie Park, NSW 2113. www.sanofi.com.au. MAT-AU-2101642.
References
- Wiviott SD, et al. Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: a PROVE IT-TIMI 22 substudy. J Am Coll Cardiol 2005;46:1411–1416.
- Cannon CP, et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med 2015;372:2387–2397.
- Mach F et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41(1):111–188.
- Schwartz G, et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N Engl J Med 2018;379:2097–2107.
- Goodman SC et al. Effects of Alirocumab on Cardiovascular Events After Coronary Bypass Surgery. J Am Coll Cardiol 2019;74:1177–1186.
- Ray KK et al. Effects of alirocumab on cardiovascular and metabolic outcomes after acute coronary syndrome in patients with or without diabetes: a prespecified analysis of the ODYSSEY OUTCOMES randomised controlled trial. Lancet Diabetes Endocrinol 2019;7(8):618–628
- Jukema JW et al. Alirocumab in Patients With Polyvascular Disease and Recent Acute Coronary Syndrome: ODYSSEY OUTCOMES Trial. J Am Coll Cardiol 2019;74:1167–1176
- Redel-Traub et al. J Am Coll Cardiol 2021;77:7 (Abstract).
- Nordestgaard BG, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: Consensus Statement of the European Atherosclerosis Society. Eur Heart J 2013;34:3478–3490.
- Szarak B, et al. Lipid Testing, Lipid-Modifying Therapy, and PCSK9 (Proprotein Convertase Subtilisin-Kexin Type 9) Inhibitor Eligibility in 27 979 Patients With Incident Acute Coronary Syndrome. Circ Cardiovasc Qual Outcomes 2021;14:e006646.
- Brieger D et al. Intensive lipid-lowering therapy in the 12 months after an acute coronary syndrome in Australia: an observational analysis. MJA 2019;210:80–85.
- Schubert J, et al. Low-density lipoprotein cholesterol reduction and statin intensity in myocardial infarction patients and major adverse outcomes: a Swedish nationwide cohort study. Eur Heart J 2021;42(3):243–252.
- Praluent PBS listing available at pbs.gov.au
- Praluent® Product Information, January 2020
Date of preparation September 2021.