In a recent virtual educational meeting, Professor Shaun Goodman (Associate Head in the Division of Cardiology at St. Michael’s Hospital and University of Toronto) and Professor David Hare (Senior Cardiologist and Director of Secondary Prevention and Heart Failure Services at Austin Health and Director of the Melbourne Lipid Centre) discussed individual risk-based guidance around target LDL-C levels and what can be achieved in real-world practice.
Prof Goodman presented the latest clinical evidence supporting LDL-C lowering strategies that reduce the risk of cardiovascular events in atherosclerotic cardiovascular disease (ASCVD), and Prof Hare shared his experience from an Australian perspective, including a symptomatic ASCVD case study from his clinical practice.
Safety of life-long LDL-C lowering3
Prof Goodman argued for the safety of very low LDL-C levels using data in patients with heterozygous hypobeta-lipoproteinaemia. These individuals have a lifelong low total cholesterol (<1.0 mmol/L), but have overall excellent health and above-average life expectancy (due to relative absence of ASCVD).3 He explained that approximately 25% of cholesterol in humans is localised to the brain and produced by local synthesis.4 Since cholesterol is required for the functioning of all cells, this concentration in the brain is relevant when discussing lipid lowering therapy; however, Prof Goodman pointed out that it is unlikely that monoclonal antibodies cross the blood-brain barrier.5
The addition of PCSK9 inhibitors to lipid lowering therapy helps achieve low LDL-C levels
Prof Goodman shared an intention-to-treat (ITT) analysis from the ODYSSEY OUTCOMES trial showing the mean LDL-C levels of patients treated on maximally tolerated statins plus placebo or alirocumab.1 At Month 4, the alirocumab group had a mean LDL-C of 1.02 mmol/L vs 2.41 mmol/L in the placebo group,1 which gradually increased in both study arms, to 1.72 mmol/L and 2.67 mmol/L in the alirocumab and placebo groups, respectively by Month 48 (p value not reported).1 Prof. Goodman offered his thoughts on the steady increase in LDL-C over this time: “There are a number of factors that could contribute to this upwards trend in the graph. Patient adherence, discontinuation, switching patients between study arms, background changes in statin dose – these are just some examples”. Prof Goodman pointed out that the on-treatment analysis showed a more consistent reduction in LDL-C throughout the study.1
A post-hoc on-treatment subgroup analysis from Prof Goodman’s own study group6 showed that patients had stable background lipid-modifying therapy, which demonstrated that there was sustained LDL-C lowering over time.6
Lowering of LDL-C showed a greater benefit in high-risk patients
In addition to the reduction in LDL-C levels, the ODYSSEY OUTCOMES trial1 found that post-ACS patients (n=18,924) with elevated LDL-C levels despite high-intensity or maximal tolerated dose of statins randomised to alirocumab demonstrated a lower risk of recurrent ischaemic cardiovascular events (death from coronary heart disease, nonfatal myocardial infarction, fatal or nonfatal ischemic stroke, or unstable angina requiring hospitalisation) compared to those randomised to placebo (9.5% in alirocumab group versus 11.1% in the placebo group; HR 0.85, 95% CI 0.78–0.93; p<0.001 over a median 2.8-year follow-up). To prevent one primary end-point event, 49 patients (95%; CI 28 to 164) would need to be treated for four years, based on a 4-year Kaplan-Meier estimate.1
Prof Goodman presented a pre-specified analysis7 of ODYSSEY OUTCOMES supporting the use of alirocumab in elderly patients (age ≥65 years), a high-risk group in the post-acute coronary syndrome (ACS) population. The findings showed that, irrespective of age, the addition of alirocumab improved CV outcomes in elderly patients, with the oldest patients seeing the greatest absolute benefit (post hoc analysis: 75 years NNT3 years ~26; 85 years NNT3 years ~12).7 Prof. Goodman stated that this absolute treatment benefit of alirocumab with advancing age suggested that “there is no reason to deprive older ACS patients of this treatment”.
Prof. Goodman concluded by noting that high-risk patients in the ODYSSEY OUTCOMES study achieved similar relative risk reductions in MACE to the overall population, but greater absolute risk reductions:1 in pre-specified subgroup analyses in high-risk groups of patients including patients with LDL-C ≥ 2.6 mmol/L,1 prior CABG,8 diabetes,9 and polyvascular disease10 – the relative risk reduction seen with the addition of alirocumab to high dose statins in each subgroup was consistent with the overall study population. However, the absolute risk reduction was greater in these high-risk groups than their respective comparators, and numerically greater than in the overall study population.1,8–10
Accessing PCSK9 inhibitor treatment in Australia, with an ASCVD patient case as an example
Prof David Hare shared his experience of using PCSK9 inhibitors in the Australian context through the case of a patient he has treated for 30 years. Now 72 years of age, he initially presented in 1991 at 42 years of age with angina and a family history of myocardial infarction (father at 50 years). The patient was a smoker, overweight at 92 kg/178 cm with no diabetes. Four years later he presented at the emergency department with resting angina over 20 minutes, and was found to have two occlusions on coronary angiogram.
In 1996, he underwent coronary artery bypass graft CABG and started on amlodipine 5 mg for 6 months and low-dose aspirin 100 mg. Between 1996 and 2021, he had no further symptoms of myocardial ischaemia.
Through a series of lipid lowering therapies over a number of years, his LDL-C levels were eventually lowered to 3.1 mmol/L with atorvastatin 40 mg plus strict diet and then to 2.8 mmol/L with cholestyramine (but this was poorly tolerated). From 2006, trials of tighter LDL management with ezetimibe 10 mg plus atorvastatin 80 mg or rosuvastatin 20 mg resulted in myalgia and elevated creatinine kinase.
In October 2007 the patient stopped all medications due to family circumstances. Diet lapsed and he gained weight, with a subsequent elevation of LDL-C (6.0 mmol/L). He subsequently resumed diet and medication (ezetimibe 10 mg/rosuvastatin 20 mg) and LDL-C levels were at 2.1 mmol/L in May 2008.
In July 2019 he presented with LDL-C level of 3.3 mmol/L. Ezetimibe 10 mg and rosuvastatin 40 mg resulted in an LDL-C of 2.9 mmol/L in September 2020.
Owing to the patient’s LDL-C levels, which are higher than the ESC/EAS guidelines recommended target of 1.4 mmol/L,11 Prof Hare suggested that the patient was a candidate for a PCSK9 inhibitor for further lipid-lowering treatment. He described the PBS approval process for prescribing a PCSK9 inhibitor (alirocumab), and demonstrated the use of the online tool for Praluent using this patient’s profile as an example.
An online tool to help navigate PBS application for Praluent (alirocumab)
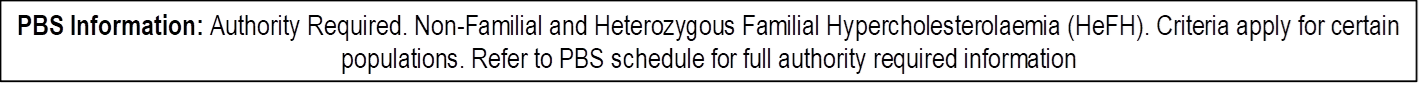
Praluent is an Authority Required PBS listed product12 for Non-Familial and Heterozygous Familial Hypercholesterolaemia (refer to PBS schedule for further criteria and restrictions). For demonstration purposes the talk focused on the Non-familial hypercholesterolemia patient depicted as:
- Symptomatic ASCVD, on diet and exercise
- Using maximum-tolerated statin + ezetimibe for >12 weeks
- LDL-C >2.6 mmol/L
- Additional CV risk factors (including severe multi-vessel CHD)
An online tool developed by Sanofi uses a simple 4-step process to assist prescribers in review of criteria ahead of the Authority application process:
- Select the PBS subsidy indication relevant to their patient.
- Enter the patient’s current lipid treatment.
- Add the patient’s LDL-C level (recorded within the last 8 weeks).
- Add other criteria (such CV risk factor)
Training and support for patients
Sanofi has partnered with a team of pharmacists to offer patient injection training support. In addition, physicians are able to apply for a training device to instruct patients during consultations. In a previous webinar, Prof Simons described his approach to patient instruction: “I just move to the other side of the desk, do the injection myself first with the training device, then get them [the patient] to do it themselves.”
Disclaimers
Praluent® is indicated to reduce the risk of cardiovascular events (myocardial infarction, stroke, unstable angina requiring hospitalisation) in adults with established cardiovascular disease, in combination with optimally dosed statins and/or other lipid-lowering therapies.13
This article was commissioned by Sanofi Australia Pty Ltd. The content is independent and based on studies and the author’s opinion. The views expressed do not necessarily reflect the views of Sanofi. Before prescribing, please review the Praluent® (alirocumab) full product information13 via the TGA website. Treatment decisions based on these data are the responsibility of the prescribing physician.
Praluent® is a registered trademark of Sanofi-Aventis Australia Pty. Ltd trading as Sanofi, ABN 31 008 558 807 Talavera Corporate Centre, Building D, 12-24 Talavera Road, Macquarie Park, NSW 2113. www.sanofi.com.au. MAT-AU-2101950
Date of preparation September 2021.
Please review full Product Information before prescribing. For full Product Information click here or contact Sanofi Medical Information on 1800 818 806.
MINIMUM PRODUCT INFORMATION: Praluent® (alirocumab (rch)) INDICATIONS Primary hypercholesterolaemia: as an adjunct to diet and exercise to reduce LDL-C in adults with primary (heterozygous familial or non-familial) hypercholesterolaemia in patients with moderate to very high cardiovascular risk: – In combination with a statin, or statin with other lipid-lowering therapies in patients unable to reach LDL-C goals with maximum tolerated dose of a statin, – alone or in combination with other lipid lowering therapies in patients who are statin intolerant or for whom a statin is contraindicated who are unable to reach LDL-C goals. Prevention of cardiovascular events: to reduce the risk of cardiovascular events (myocardial infarction, stroke, unstable angina requiring hospitalisation) in adults with established cardiovascular disease, in combination with optimally dosed statins and/or other lipid lowering therapies (see full PI). DOSAGE AND ADMINISTRATION 75 mg subcutaneously every 2 weeks or 300 mg every 4 weeks. May increase to 150 mg every 2 weeks if inadequate LDL-C response. Measure lipid levels from 4-8 weeks of initiating/titrating Praluent, to assess response and adjust dose if needed. To administer 300 mg, give two 150 mg injections consecutively at two different injection sites. Inject into thigh or abdomen or upper arm that is not tender, bruised, red or hard (rotate site). Allow to warm at room temperature (up to 25°C) for 30-40 min before injecting; do not warm in any other way. See full PI. CONTRAINDICATIONS Hypersensitivity to the active substance or to any of the excipients. PRECAUTIONS General allergic reactions, immunogenicity, very low LDL-C levels (long-term effects unknown), pregnancy (category B1), lactation, children (<18 years). Severe hepatic (Child-Pugh C) or severe renal impairment (eGFR < 30 mL/min/1.73 m2) not studied. INTERACTIONS Not anticipated. ADVERSE EFFECTS Common adverse reactions: injection site reactions, pruritus, upper respiratory tract signs and symptoms. Others, see full PI. NAME OF SPONSOR Sanofi-Aventis Australia Pty Ltd, 12-24 Talavera Road, Macquarie Park, NSW 2113. DATE OF PREPARATION 14 January 2020. Based on Full Product Information with TGA date of approval of 17 May 2016, with most recent amendment on 10 January 2020.
References
- Schwartz G, et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N Engl J Med 2018;379:2097–2107.
- O’Keefe JH, et al. Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. J Am Coll Cardiol 2004;43:2142–2146.
- O’Keefe JH, et al. Statins, Ezetimibe, and Proprotein Convertase Subtilisin-Kexin Type 9 Inhibitors to Reduce Low-Density Lipoprotein Cholesterol and Cardiovascular Events. J Am Coll Cardiol 2017;119:565–571.
- Bjorkhem I, Meaney S. Brain cholesterol: long secret life behind a barrier. Arterioscler Thromb Vasc Biol 2004;24:806–815.
- Alkindi M, et al. Monoclonal Antibodies for the Treatment of Hypercholesterolemia: Targeting PCSK9. Can J Cardiol 2016;32:1552–1560.
- Goodman S, et al. Sustained Low-Density Lipoprotein Cholesterol Lowering With Alirocumab in ODYSSEY OUTCOMES. J Am Coll Cardiol 2019;75:448–451.
- Sinnaeve PR, et al. Effect of alirocumab on cardiovascular outcomes after acute coronary syndromes according to age: an ODYSSEY OUTCOMES trial analysis. Eur Heart J 2019; 41(24:2248–2258.
- Goodman SC et al. Effects of Alirocumab on Cardiovascular Events After Coronary Bypass Surgery. J Am Coll Cardiol 2019;74:1177–1186.
- Ray KK et al. Effects of alirocumab on cardiovascular and metabolic outcomes after acute coronary syndrome in patients with or without diabetes: a prespecified analysis of the ODYSSEY OUTCOMES randomised controlled trial. Lancet Diabetes Endocrinol 2019;7(8):618–628
- Jukema JW et al. Alirocumab in Patients With Polyvascular Disease and Recent Acute Coronary Syndrome: ODYSSEY OUTCOMES Trial. J Am Coll Cardiol 2019;74:1167–1176
- Mach F, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41(1):111–188.
- Praluent PBS listing available at pbs.gov.au
- Praluent® Product Information, January 2020