Ongoing analysis of data from the ODYSSEY OUTCOMES trial continues to shed light on the benefits of lowering elevated LDL-cholesterol (LDL-C) levels with the PCSK9 inhibitor alirocumab in patients at high risk of cardiovascular (CV) events.1-8 In this article, Professor Gerald Watts from the Royal Perth Hospital gives his impressions of the data. He also describes how a shared decision-making approach can lead to better adherence for optimal outcomes.
“The benefits in the ODYSSEY OUTCOMES trial were seen across pre-specified subgroups, including people with diabetes, impaired kidney disease, older and younger patients, and male and female patients.1-5 So, it’s a true effect that supports the notion of identifying high-risk people with elevated LDL-C, lowering their LDL-C and sustaining the reduction,” says Prof. Watts. “We know that reducing the burden of LDL-C over time is important. The longer we do that, the greater the benefit,” he explains.
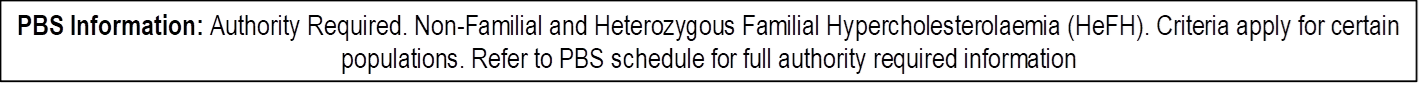
“PCSK-9 monoclonal antibodies will bring a large proportion of patients below an LDL-C target of <1.8 mmol/L. A PCSK-9 monoclonal antibody should be considered for referred patients with known CV disease and an LDL-C level above the PBAC-required threshold of 2.6 mmol/L on a maximal tolerated dose of statin plus ezetimibe,” says Prof. Watts. “If the patient wishes to pay for it privately, you can disregard the LDL-C threshold and treat the patient to a target of around 1.4 mmol/L,” he explains.
“There is also a group of people who cannot get to the required LDL-C thresholds due to statin intolerance. For those with statin intolerance and at high risk of CV events, prescribers should consider a PCSK-9 monoclonal antibody in addition to ezetimibe or other lipid-lowering therapy,” says Prof. Watts.
Insights from ODYSSEY OUTCOMES data analysis
The primary results of the ODYSSEY OUTCOMES trial were published in 2018.1 The randomised, double-blind, placebo controlled trial was conducted in 18,924 patients who had experienced an acute coronary syndrome (ACS) in the previous 1 – 12 months and whose atherogenic lipoproteins remained elevated despite high-dose statins. Patients were randomised to alirocumab (75 mg subcutaneously every two weeks) or placebo and the dose was adjusted to achieve a target low-density lipoprotein cholesterol (LDL-C) level of 0.6 to 1.3 mmol/L. The primary composite endpoint was death from coronary heart disease, nonfatal myocardial infarction, fatal or nonfatal ischaemic stroke or unstable angina requiring hospitalisation.
Over a median follow-up of 2.8 years, patients receiving alirocumab achieved a marked reduction in LDL-C levels and a lower risk of recurrent ischaemic cardiovascular events compared to those on placebo (hazard ratio, 0.85; 95% CI, 0.78–0.93, P<0.001).1
The incidence of adverse events was similar in the two groups, with the exception of local injection-site reactions (3.8% in the alirocumab group vs. 2.1% in the placebo group).
Further analyses of the data and other trials published throughout 2020 provide clinicians with an even greater understanding of the benefits of alirocumab in patients at high risk of cardiovascular events, including effects in males versus females,2 long-term lipid lowering effects,6 and proportion of patients who can achieve target LDL-C levels.7
Cardiovascular outcomes improved irrespective of sex, according to a pre-specified sub-group analysis of the data.1,2 The analysis found that women were older, had slightly higher LDL-C levels, more diabetes and hypertension, but smoked less than the male study population. They were also less likely to have had an ST elevation myocardial infarction or percutaneous interventions. However, there was no significant difference in the hazard ratios for major cardiovascular events and death between men and women (MACE: p value for sex-treatment interaction = 0.35, CHD death: p value for sex-treatment interaction = 0.52). Adverse events were more frequent in women than in men, but there were no differences between alirocumab and placebo. The authors conclude, “In patients with recent ACS, alirocumab improves cardiovascular outcomes irrespective of sex.”
Lipid lowering was sustained over at least three years with alirocumab, as shown in an examination of LDL-C levels in patients who had remained on sustained and consistent lipid lowering therapy over the three-year follow-up period and had all LDL-C measurements (n=1,672).6 The authors reported “a consistent and sustained reduction in median LDL-C levels with alirocumab, from month 1 (first post-randomisation evaluation; absolute 47 mg/dL and relative 53% reductions vs. placebo) through month 36 (absolute 55 mg/dL and relative 62% reductions vs. placebo) and through 3 years.” They note that this maintenance of LDL-C lowering is similar to previous studies of shorter duration.
An LDL-C target of less than 1.3 mmol/L (50 mg/dL) may be reasonable after ACS, according to a propensity score-matched analysis of the ODYSSEY OUTCOMES trial.9 The analysis classified patients on alirocumab into one of three pre-specified LDL-C categories after four months of treatment: <25 mg/dL, 25 – 50 mg/dL, and >50 mg/dL. Within each category, major adverse cardiovascular events (MACE) was compared with patients on placebo using a 1:1 propensity score match on demographic, clinical and adherence variables. The analysis showed that hazard ratios for MACE were similar in those who achieved LDL-C <25 mg/dL and those who achieved 25–50 mg/dL, whereas patients with LDL-C >50 mg/dL had less benefit from treatment. The authors concluded, “These data suggest that an LDL-C target of less than 50 mg/dL [1.3mmol/L] may be reasonable after ACS and is essentially congruent with new ESC/EAS guidelines.”
Achieving clinically significant LDL-C reductions in a real-world setting, was evaluated in the ODYSSEY APPRISE.10 This was a separate prospective, single-arm open-label study investigating the safety and efficacy of alirocumab in a real-life setting in patients at higher risk of cardiovascular events with severe hypercholesterolaemia not adequately controlled on maximally tolerated doses of statins with or without other lipid lowering therapies.
Patients received alirocumab (75 mg or 150 mg every two weeks, with dose adjustments based on physician’s judgement). The study found that alirocumab was generally well tolerated and resulted in clinically significant LDL-C reductions.
Over a mean treatment duration of 72.4 weeks, the overall incidence of treatment-emergent adverse events was 71.6% with common TEAEs including nasopharyngitis (7.8%), myalgia (7.1%), headache (6.2%) and influenza (5.3%). At Week 12, LDL-C was reduced by a mean 54.8% (20.1% SD) from baseline. LDL-C was reduced below 1.8 mmol/L and/or by ≥50% reduction from baseline in 64.7% of patients with heterozygous familial hypercholesterolaemia and 77.4% of patients with non-familial hypercholesterolaemia. Reductions were maintained for the trial duration.
Persistence to effective therapy is the key to good outcomes
“It’s important to remind patients to continue their statin and ezetimibe, unless there is an intolerance” says Prof. Watts. “Some people expect that once they start the injection they can stop their statin. It’s quite important to make it clear upfront that the efficacy in clinical trials is for adding the PCSK-9 inhibitor to a statin,” he explains.
“You’re going to get the greatest return on investment (in terms of cost of medication and patient effort to inject fortnightly) if you continue on the high-dose statin and another high dose cholesterol lowering agent (being ezetimibe). If the person is intolerant to statins, it’s fundamental that patients are told the importance of taking ezetimibe,” explains Prof. Watts.
Shared decision making is “absolutely critical”
Prof. Watts strongly believes that only shared decision making will achieve optimal patient outcomes. “Shared decision making and involving the patient in management is absolutely critical,” he says. “You need to spend time explaining to the patient the rationale for therapy, how to administer it, possible treatment side effects, and the return on investment they can expect, particularly if they are paying for it privately.”
Good communication with the patient’s general practitioner (GP) is also essential, explains Prof. Watts. “It’s quite important to get this right because initially many GPs were not comfortable to prescribe a repeat prescription for a PCSK-9 inhibitor. To get around this, work with the GP…it’s important to follow up with good communication in a letter to say that the patient should continue therapy and to check the effectiveness and safety of the therapy every 4-6 months,” he says.
“You don’t ‘put’ patients on therapy,” says Prof. Watts. “You ‘offer’ it and discuss the rationale for therapy in a shared decision setting.”
Disclosure
This article was commissioned by Sanofi Australia Pty Ltd. Any views expressed in the article are those of the expert alone and do not necessarily reflect the views of the sponsor. Before prescribing, please review the [Product] product information via the TGA website. Treatment decisions based on these data are the responsibility of the prescribing physician.
References
- Schwartz GG et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. NEJM 2018;379:2097–2107 https://www.nejm.org/doi/full/10.1056/NEJMoa1801174
- Bittner V et al. Alirocumab and cardiovascular outcomes in women after an acute coronary syndrome: An Odyssey Outcomes trial analysis. Poster Presentation. JACC 2020;75 (11):1854 https://www.jacc.org/doi/full/10.1016/S0735-1097%2820%2932481-5
- Ray KK et al. Effects of alirocumab on cardiovascular and metabolic outcomes after acute coronary syndrome in patients with or without diabetes: a prespecified analysis of the ODYSSEY OUTCOMES randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7(8):618-628. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6175384/
- Tunon J et al. Effect of alirocumab on major adverse cardiovascular events according to renal function in patients with a recent acute coronary syndrome: a prespecified analysis from the ODYSSEY OUTCOMES randomized clinical trial. Eur Heart J 2020;41(42):4114–4123. https://academic.oup.com/eurheartj/article/41/42/4114/5895197
- Sinnaeve PR et al. Effect of alirocumab on cardiovascular outcomes after acute coronary syndromes according to age: and ODYSSEY OUTCOMES trial analysis. Eur Heart J 2020;41(24):2248–2258. https://academic.oup.com/eurheartj/article/41/24/2248/5626150
- Goodman S et al. Sustained low-dose lipoprotein cholesterol lowering with alirocumab in ODYSSEY OUTCOMES. JACC 2020;75(4);48–51 https://www.jacc.org/doi/full/10.1016/j.jacc.2019.11.030
- Landmesser U et al. Achievement of new European dyslipidemia-guideline low-density lipoprotein cholesterol treatment goals after acute coronary syndrome: insights from Odyssey Outcomes. JACC 2020;75(11):1978 https://www.jacc.org/doi/full/10.1016/s0735-1097%2820%2932605-x
- Mach F et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The taskforce for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2019; 41:111–188. https://academic.oup.com/eurheartj/article/41/1/111/5556353
- Schwartz GG et al. Low-density lipoprotein cholesterol <50 mg/dL is an appropriate target after acute coronary syndrome: propensity score-matched analysis of the ODYSSEY OUTCOMES trial. Eur Heart J. 2020;41(Suppl.2);ehaa946.1736 https://doi.org/10.1093/ehjci/ehaa946.1736
- Gaudet D et al. Safety and efficacy of alirocumab in a real-life setting: the ODYSSEY APPRISE study. JACC 2020;75(11):1958 https://www.jacc.org/doi/full/10.1016/s0735-1097%2820%2932585-7
Praluent® is a registered trademark of Sanofi-Aventis Australia Pty. Ltd trading as Sanofi, ABN 31 008 558 807 Talavera Corporate Centre, Building D, 12-24 Talavera Road, Macquarie Park, NSW 2113. www.sanofi.com.au. MAT-AU-2101950
Date of preparation October 2021.
Please review full Product Information before prescribing. For full Product Information click here or contact Sanofi Medical Information on 1800 818 806.
MINIMUM PRODUCT INFORMATION: Praluent® (alirocumab (rch)) INDICATIONS Primary hypercholesterolaemia: as an adjunct to diet and exercise to reduce LDL-C in adults with primary (heterozygous familial or non-familial) hypercholesterolaemia in patients with moderate to very high cardiovascular risk: – In combination with a statin, or statin with other lipid-lowering therapies in patients unable to reach LDL-C goals with maximum tolerated dose of a statin, – alone or in combination with other lipid lowering therapies in patients who are statin intolerant or for whom a statin is contraindicated who are unable to reach LDL-C goals. Prevention of cardiovascular events: to reduce the risk of cardiovascular events (myocardial infarction, stroke, unstable angina requiring hospitalisation) in adults with established cardiovascular disease, in combination with optimally dosed statins and/or other lipid lowering therapies (see full PI). DOSAGE AND ADMINISTRATION 75 mg subcutaneously every 2 weeks or 300 mg every 4 weeks. May increase to 150 mg every 2 weeks if inadequate LDL-C response. Measure lipid levels from 4-8 weeks of initiating/titrating Praluent, to assess response and adjust dose if needed. To administer 300 mg, give two 150 mg injections consecutively at two different injection sites. Inject into thigh or abdomen or upper arm that is not tender, bruised, red or hard (rotate site). Allow to warm at room temperature (up to 25°C) for 30-40 min before injecting; do not warm in any other way. See full PI. CONTRAINDICATIONS Hypersensitivity to the active substance or to any of the excipients. PRECAUTIONS General allergic reactions, immunogenicity, very low LDL-C levels (long-term effects unknown), pregnancy (category B1), lactation, children (<18 years). Severe hepatic (Child-Pugh C) or severe renal impairment (eGFR < 30 mL/min/1.73 m2) not studied. INTERACTIONS Not anticipated. ADVERSE EFFECTS Common adverse reactions: injection site reactions, pruritus, upper respiratory tract signs and symptoms. Others, see full PI. NAME OF SPONSOR Sanofi-Aventis Australia Pty Ltd, 12-24 Talavera Road, Macquarie Park, NSW 2113. DATE OF PREPARATION 14 January 2020. Based on Full Product Information with TGA date of approval of 17 May 2016, with most recent amendment on 10 January 2020.