A new and revised clinical care standard for acute stroke has been released to try address ongoing gaps in care such as underuse of thrombolysis and stroke units.
Published by the by the Australian Commission on Safety and Quality in Health Care, the update to the standards first released in 2015 includes revisions to reflect trends such as increasing use of endovascular thrombectomy.
The standards’ authors say that despite some improvements seen in stroke care following the first set of standards, there is still a need for Australia to catch up with other countries in areas such as provision of timely thrombolysis.
“Many [acute stroke] patients still do not receive any form of potentially lifesaving reperfusion therapy [and] the number of stroke units in Australia has increased, but patients spend less time in stroke units than they should,” they write
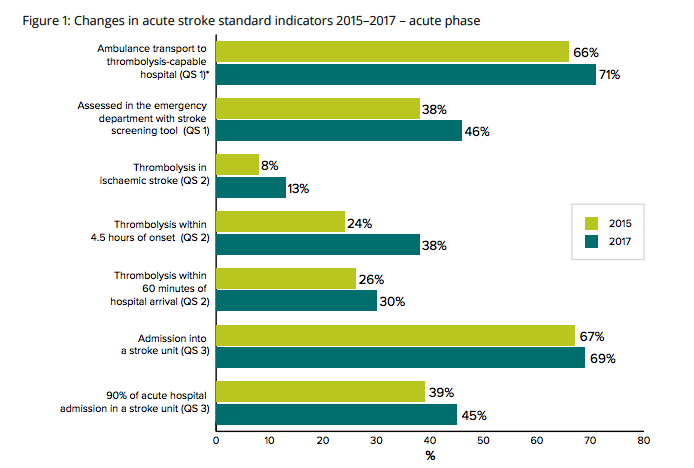
They note that the proportion of patients receiving thrombolysis has almost doubled, from 8% to 13% since the previous standards were released, and endovascular thrombectomy now provides an alternative option to thrombolysis for reperfusion treatment.
“Nonetheless, there is much still to be done to improve the care of patients with an acute stroke. Overall rates of thrombolysis remain low, fewer than 50% of patients spend most of their acute hospital stay within a stroke unit and more than 30% of patients do not receive a physiotherapy assessment in the first 48 hours of admission.”
 The standards include 17 quality indicators that can be monitored across seven key areas of care (see below):
The standards include 17 quality indicators that can be monitored across seven key areas of care (see below):
“Clinicians and health service organisations can use these indicators to monitor their implementation of the care described each quality statement and the clinical care standard as a whole,” the authors suggest.
Many of the major changes in the clinical care standard have been to align them with the Stroke Foundation’s Clinical Guidelines for Stroke Management and the Australian Stroke Clinical Registry (AuSCR).
The standard has been produced by a working group that included stroke neurologists Professor Christopher Levi, Dr Helen Castley and Dr Jim Jannes and stroke physicians Professor Richard Lindley and Dr Rohan Grimley.
Quality Statements:
- Early assessment: A person with suspected stroke is immediately assessed at first contact using a validated stroke screening tool, such as the F.A.S.T. (Face, Arm, Speech and Time) test.
- Time-critical therapy: A patient with ischaemic stroke for whom reperfusion treatment is clinically appropriate, and after brain imaging excludes haemorrhage, is offered a reperfusion treatment in accordance with the settings and time frames recommended in the Clinical Guidelines for Stroke Management.
- Stroke unit care: A patient with stroke is offered treatment in a stroke unit as defined in the National Acute Stroke Services Framework.
- Early rehabilitation: A patient’s rehabilitation needs and goals are assessed by staff trained in rehabilitation within 24–48 hours of admission to the stroke unit. Rehabilitation is started as soon as possible, depending on the patient’s clinical condition and their preferences.
- Minimising risk of another stroke: A patient with stroke, while in hospital, starts treatment and education to reduce their risk of another stroke.
- Carer training and support: A carer of a patient with stroke is given practical training and support to enable them to provide care, support and assistance to a patient with stroke.
- Transition from hospital care: Before a patient with stroke leaves the hospital, they are involved in the development of an individualised care plan that describes the ongoing care that the patient will require after they leave hospital. The plan includes rehabilitation goals, lifestyle modifications and medicines needed to manage risk factors, any equipment they need, follow-up appointments, and contact details for ongoing support services available in the community. This plan is provided to the patient before they leave hospital, and to their general practitioner or ongoing clinical provider within 48 hours of discharge.