Shrinking or non-existent Medicare rebates mean cardiology patients are now having to pay hundreds and sometimes thousands of dollars in gap fees for “standard of care” radiology tests, advocacy groups say.
Patients now face up to $2400 upfront costs and $775 out of pocket costs for tests such as coronary calcium scoring CT, echocardiogram and combined stress and rest study with SPECT, the Senate’s Community Affairs Reference Committee was told at a public hearing in Brisbane on 13 December.
Similarly, stroke patients faced upfront costs of more than $3,000 and gap fees of $586 for imaging tests such as CT, MRI, and ultrasound because Medicare rebates have been frozen since 1998, according to figures presented by the Australian Diagnostic Imaging Association to the inquiry into the availability and accessibility of diagnostic imaging equipment around Australia.
High out of pocket costs also arose because the Medicare system wasn’t keeping pace with imaging technology and rebates had not been approved for many tests that are now considered the basic standard of care, the Association said.
“Patients often require more than one radiology service for diagnosis, treatment and monitoring, meaning that patients pay thousands of dollars upfront and are left hundreds of dollars out of pocket,” the ADIA said in its submission to the inquiry
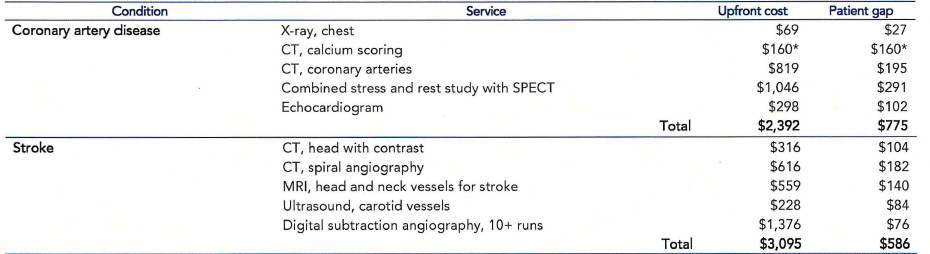
Source: ADIA
Patients can expect gap fees for scans to double in costs over the next decade unless action is taken to unfreeze the Medicare rebates for imaging, the hearing was told.
There was also a need to reform the slow and outdated system of approvals for Medicare rebates for radiology services, with the Medicare Services Advisory Committee (MSAC), taking three or more years to consider applications, said the ADIA.
By the time its rulings come out, technology had already moved on to other tests that were standard practice overseas, it said.
“To stop patients missing out on clinically appropriate services recommended by their doctor, the government should review the process and criteria that MSAC uses to determine its recommendations to the Government for radiology services. The guiding principle should be that services referred for by specialists at arm’s length in significant volumes (i.e. services that have become ‘standard of care’) should be listed on Medicare and available to all Australians,” it recommended.
The claims were backed up by the Australian Society for Ultrasound in Medicine, which includes cardiologists among its members.
“The Medicare rebate hasn’t changed for ultrasound in over 20 years, restricting services in all specialties, which in turn affects patient management,” said the society’s president, Professor George Condous.
“This relates to many patients not attending appointments due to the fee or gap incurred, which is crucial to the management of their disease, often then creating a burden on Medicare to support the patient, who then subsequently needs additional care because they may present with a later or more advanced disease stage,” he told a public hearing in December.