With no molecular biomarkers to predict immunotherapy response in metastatic melanoma, Sydney researchers have found that a combination of standard clinical measures such as baseline blood parameters help predict overall survival.
In what they say could be a simple and useful tool for clinical decision making, researchers at the Melanoma Institute Australia, University of Sydney have developed a risk calculator for patient responses to anti-PD1 and anti-CTLA-4 therapy.
Presenting their findings at ASCO 2019 in Chicago, the researchers said there had previously been studies into how factors such as low lymphocyte count and high neutrophil count may be associated with shorter overall survival in metastatic melanoma, but these factors had only been studied individually and had not been validated.
They therefore explored the associations of various clinical and molecular variables in 786 metastatic melanoma patients: 343 patients treated with anti-PD-1 checkpoint inhibitors (and a further 104 for validation) and 229 patients treated with ipilimumab and anti-PD-1 therapies (and 110 for validation)
Except for age and elevated LDH, few of the individual patient or disease characteristics such as ECOG score and mutation status were strongly associated with outcomes in any of the cohorts.
However by combining the results of various routinely collected clinical factors such as primary site, brain mets and monocyte count, the researchers found that these provided a good predictive model for progression free survival (AUC = 0.72) and overall survival in the PD-1 cohort (AUC = 0.74), and also in the ipilimumab + PD-1 cohort.
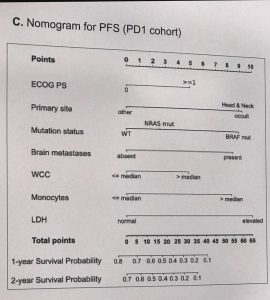 By assigning points to the various clinical factors, risk calculator nomograms were developed for Progression Free Survival and Overall Survival for both cohorts.
By assigning points to the various clinical factors, risk calculator nomograms were developed for Progression Free Survival and Overall Survival for both cohorts.
For the PD-1 cohorts the variables included ECOG score, mutational status, brain mets, neutrophils, monocytes, NLR and LDH. A novel predictive factor of basophil count was associated with good outcomes in the ipilimumab + PD-1 cohort.
In the PD-1 cohort, patients who had high risk scores from the nomogram had overall survival rates at 24 months of below 25%, compared to around 75% for those with low risk scores.
“A combination of routinely collected clinical factors are highly predictive of outcome in metastatic melanoma patients treated with PD-1 and ipilimumab and PD-1 … Such tools may be practical, cheap and valuable for clinical decision making,” they concluded.